Sleep Restriction Therapy: How to Reset Insomnia Patterns for Good
 Dec, 7 2025
Dec, 7 2025
For years, people with insomnia have been told to sleep more. But what if the problem isn’t that you’re not sleeping enough-it’s that you’re spending too much time in bed awake? That’s the counterintuitive idea behind sleep restriction therapy, a proven method to break the cycle of chronic insomnia without pills.
Why More Time in Bed Makes Insomnia Worse
If you’ve been lying in bed for eight hours and only sleeping five, your brain starts to associate your bed with frustration, not rest. You check the clock. You toss and turn. You worry about tomorrow. Over time, your bed becomes a place of anxiety, not sleep. This is called conditioned arousal-and it’s one of the main reasons insomnia sticks around. Sleep restriction therapy flips the script. Instead of trying to force more sleep, it limits your time in bed to match how much you’re actually sleeping. It sounds harsh. It feels worse at first. But it works because it rebuilds your sleep drive from the ground up. Research from the American Academy of Sleep Medicine shows that CBT-I (Cognitive Behavioral Therapy for Insomnia), which includes sleep restriction, is the first-line treatment for chronic insomnia-more effective than sleeping pills and with lasting results. A 2023 study found that 78% of people who completed sleep restriction therapy still had better sleep six months later. Compare that to medication, where only 32% kept the gains after stopping.How Sleep Restriction Therapy Actually Works
This isn’t about going to bed later or skipping naps. It’s a structured, science-backed protocol with clear steps:- Track your sleep for 7 days. Use a sleep diary. Write down when you get into bed, when you fall asleep, when you wake up, and any nighttime awakenings. Don’t guess-record it every morning.
- Calculate your average total sleep time. Add up all the hours you slept over the week and divide by seven. If you slept 5, 5.5, 4.5, 6, 5, 5.5, and 6 hours, your average is about 5.4 hours. That’s your starting point.
- Set your time-in-bed limit. You now get to spend only that amount of time in bed-no more. If your average is 5.4 hours, you get 5.5 hours in bed. That might mean going to bed at 1 a.m. and waking at 6:30 a.m., even if you feel exhausted.
- Stick to a fixed wake time. No exceptions. Not on weekends. Not when you’re tired. This is the anchor that resets your internal clock.
- Wait for sleep efficiency to improve. Sleep efficiency is the percentage of time you spend asleep while in bed. If you’re in bed for 5.5 hours and sleep 5 hours, your efficiency is 91%. Once you hit 85-90% for three nights in a row, you add 15 minutes to your time in bed.
- Gradually increase until you hit 7-8 hours. Most people reach their ideal sleep window in 6 to 8 weeks. The goal isn’t to sleep more-it’s to sleep better, faster, and more consistently.
What Happens in the First Week?
The first few days are the hardest. You’ll feel tired. Maybe even foggy. That’s normal. Your body isn’t used to being so tightly scheduled. But this fatigue isn’t dangerous-it’s the signal your brain needs to reset. A 2023 survey of over 1,200 people using sleep restriction therapy found that 68% reported significant daytime sleepiness in the first two weeks. But by week three, 76% said their sleep quality had improved. The key? Consistency. People who stuck to their wake time-even on weekends-were twice as likely to succeed. Don’t nap. Even a 20-minute nap can undo progress. Your sleep drive needs to build up. Napping steals that pressure. If you’re struggling, try walking outside in daylight, drinking cold water, or doing light activity. Don’t lie down.Why It Works Better Than Pills
Sleeping pills might help you fall asleep faster, but they don’t fix the underlying problem. Benzodiazepines and Z-drugs reduce sleep onset latency by about 20-30 minutes on average-but they come with risks: dependency, grogginess the next day, and rebound insomnia when you stop. Sleep restriction therapy doesn’t just help you sleep-it reteaches your brain how to sleep. A 2023 meta-analysis showed that people using SRT reduced their time spent awake in bed by 47% more than those just doing sleep hygiene. And the benefits keep growing. A study in postmenopausal women found SRT improved sleep efficiency by 22.7%, while medication only managed 15.3%-and relapse rates were much higher with drugs. One Reddit user, SleepSeeker89, wrote: “After three weeks of strict SRT, my sleep efficiency jumped from 68% to 89%. I fall asleep in 15 minutes instead of hours.” That’s not luck. That’s biology. Your body responds to structure.Who Should Avoid Sleep Restriction Therapy?
This isn’t for everyone. If you have severe depression, bipolar disorder, or untreated sleep apnea, you need medical supervision before starting. People who drive for a living or operate heavy machinery should be cautious-daytime sleepiness in the early phase can be dangerous. Also, if you’re already getting less than 5 hours of sleep per night, you may need to start with a slightly higher time-in-bed limit (like 5.5 hours) to avoid excessive risk. Always consult a sleep specialist if you’re unsure. And if you have anxiety about sleep? That’s where stimulus control therapy comes in. It’s usually paired with SRT. The rule: bed is for sleep and sex only. No reading, no phone scrolling, no worrying in bed. If you’re awake for more than 20 minutes, get up, go to another room, and do something quiet until you feel sleepy. Then go back to bed.Tools and Support That Actually Help
You don’t need a therapist to start-but having one improves your odds. There are about 1,200 CBT-I-certified clinicians in the U.S. alone. Many offer virtual sessions. Digital tools are making SRT more accessible. Apps like CBT-i Coach (developed by the VA) and Sleepio have helped thousands. A 2023 VA study showed 72% user satisfaction with CBT-i Coach. In October 2023, the FDA approved Somryst, the first digital therapy for insomnia that includes sleep restriction. It’s now available by prescription. If you’re going solo, use a free sleep diary template from the Sleep Foundation or a simple spreadsheet. Track your time in bed, sleep time, and wake time every day. Use a timer for your wake-up. Set a reminder to go to bed. No excuses.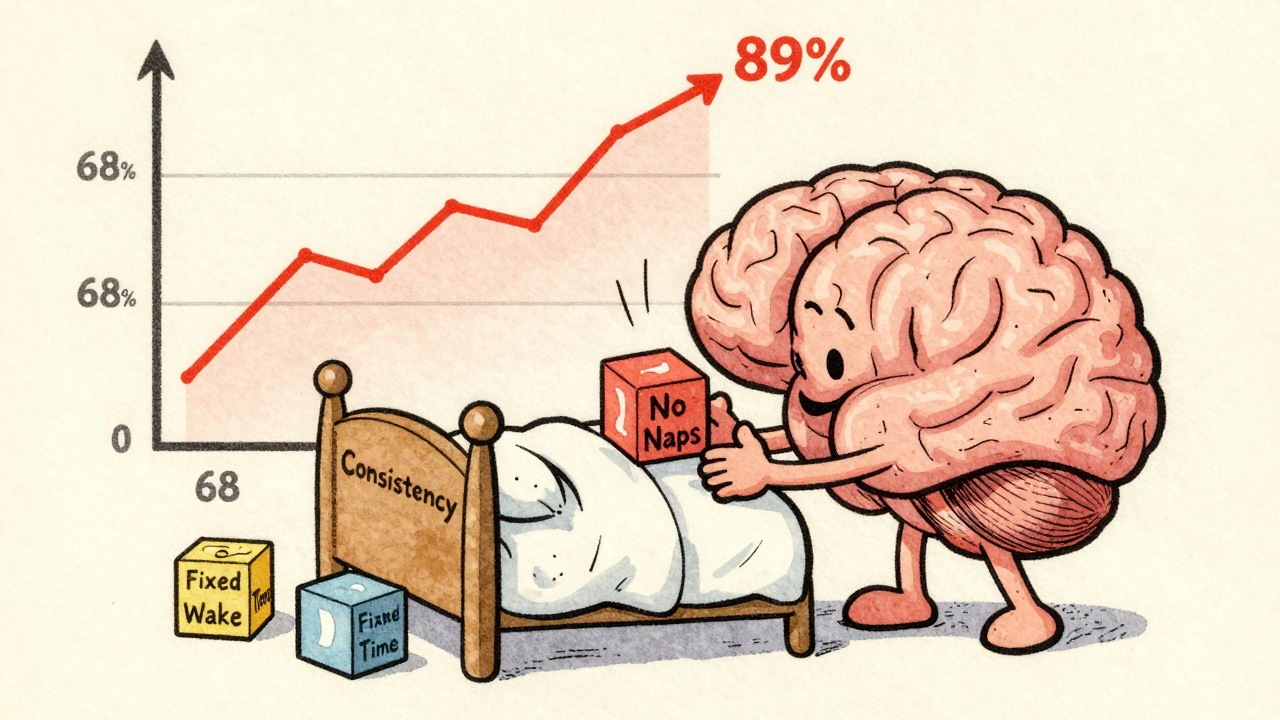
The Long-Term Payoff
The biggest myth about sleep restriction therapy is that it’s a short-term fix. It’s not. It’s a permanent reset. Dr. Colleen Carney, a leading sleep researcher, says SRT is “the most durable insomnia treatment available.” Unlike medication, where effects fade after stopping, SRT’s benefits often grow stronger over time. Why? Because you’re not relying on a chemical. You’re rebuilding a habit. A 2023 study from Sleepstation.org.uk followed people for a year. Of those who completed SRT, 68% still had better sleep. Only 29% of medication users did. This isn’t about sleeping more. It’s about sleeping better. It’s about waking up feeling like you’ve actually rested-not just passed out.What to Do If It’s Not Working
If after 6 weeks you’re not seeing improvement, ask yourself:- Did I stick to my wake time every single day-even weekends?
- Did I avoid naps completely?
- Did I use a sleep diary accurately?
- Did I combine it with stimulus control?

Taya Rtichsheva
December 8, 2025 AT 19:21Christian Landry
December 9, 2025 AT 01:56Noah Raines
December 9, 2025 AT 09:39Katherine Rodgers
December 9, 2025 AT 13:53Lola Bchoudi
December 10, 2025 AT 11:14Katie Harrison
December 12, 2025 AT 10:51Guylaine Lapointe
December 12, 2025 AT 10:53Asset Finance Komrade
December 13, 2025 AT 20:14Mona Schmidt
December 14, 2025 AT 17:55Ruth Witte
December 16, 2025 AT 03:28Gilbert Lacasandile
December 16, 2025 AT 03:41Lauren Dare
December 17, 2025 AT 19:08