Parkinson’s Disease and Antipsychotics: How Medications Can Worsen Movement Symptoms
 Oct, 28 2025
Oct, 28 2025
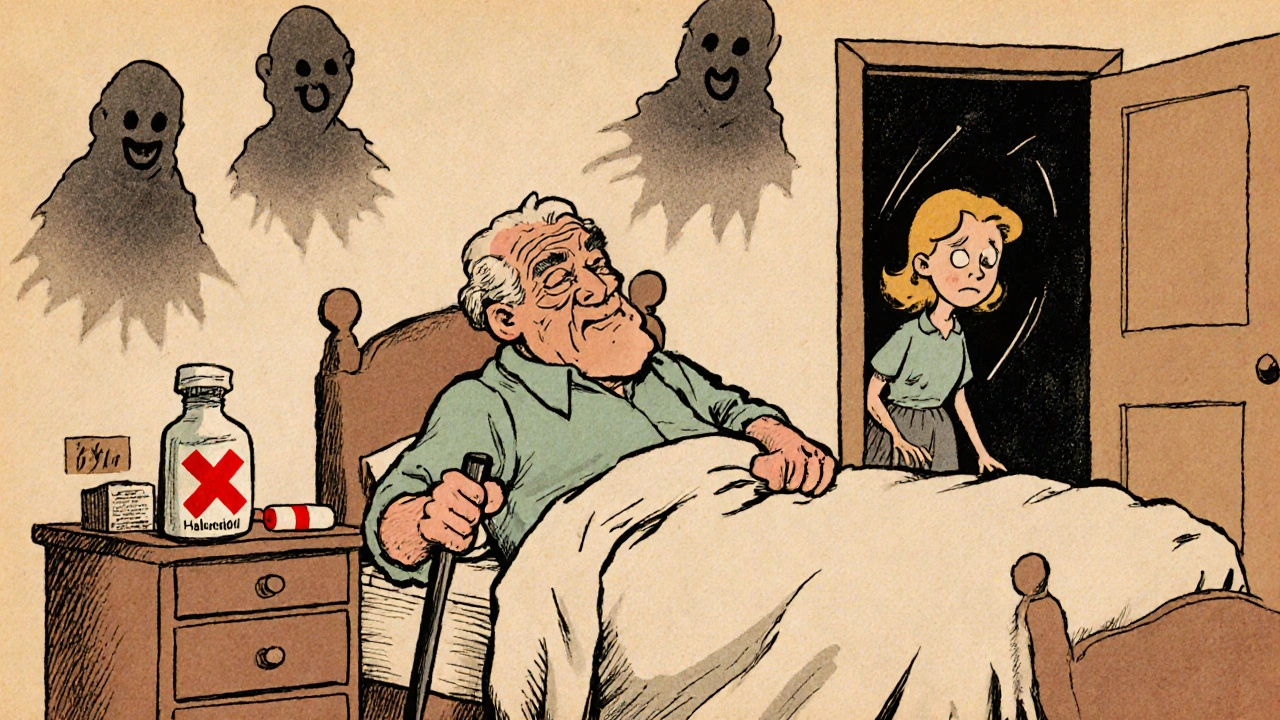
When someone with Parkinson’s disease starts seeing things that aren’t there-people in the room, shadows moving, or loved ones who have passed away-it’s terrifying. Not just for them, but for everyone around them. This is Parkinson’s disease psychosis (PDP), and it affects about 24% of people with Parkinson’s, according to the Parkinson’s Foundation. The natural urge is to treat it with an antipsychotic. But here’s the catch: most antipsychotics make the shaking, stiffness, and slowness worse. In some cases, they can turn a person who was walking with a cane into someone who can’t stand without help.
Why Antipsychotics Make Parkinson’s Worse
Parkinson’s disease is caused by the loss of dopamine-producing nerve cells in the brain. Dopamine isn’t just about mood-it’s what helps your body move smoothly. Without enough of it, you get tremors, rigid muscles, and slow movements. That’s why levodopa, a dopamine booster, is the main treatment. Antipsychotics work by blocking dopamine receptors, especially the D2 type. That’s how they reduce hallucinations and delusions in schizophrenia. But in Parkinson’s, you’re already low on dopamine. Blocking what’s left is like turning off the last bit of fuel in an engine that’s barely running. The result? Motor symptoms spike. This isn’t guesswork. It’s been known since the 1970s. A 1996 guideline from the American Academy of Neurology was one of the first to warn doctors: Don’t use standard antipsychotics in Parkinson’s patients. The problem is, many still do-because they don’t know the alternatives.The Worst Offenders: First-Generation Antipsychotics
Not all antipsychotics are created equal. First-generation antipsychotics (FGAs), also called typical antipsychotics, are the most dangerous for Parkinson’s patients. These include:- Haloperidol (Haldol)
- Fluphenazine
- Chlorpromazine
The Safer Options: Clozapine and Quetiapine
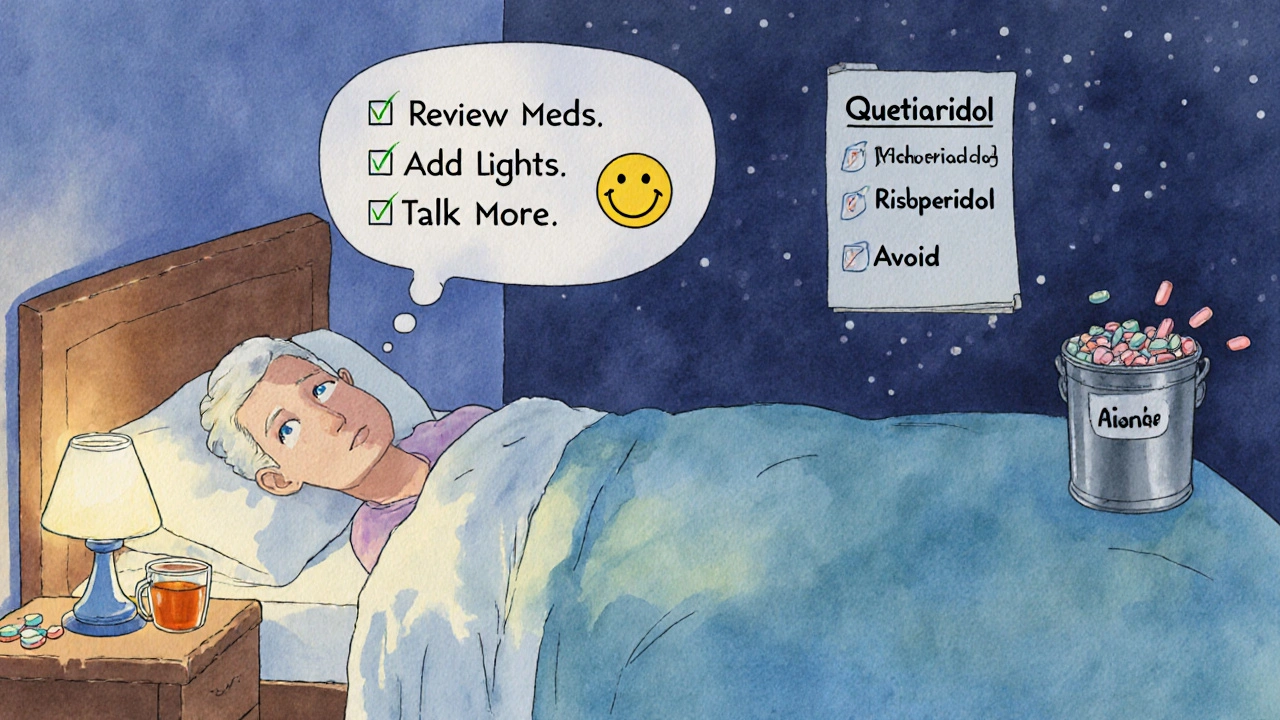
There are two antipsychotics that don’t wreck motor function-when used correctly. Clozapine is the gold standard. It was approved by the FDA for Parkinson’s psychosis in 2016. It blocks dopamine receptors only weakly (40-60% occupancy) and also works on serotonin receptors, which helps calm psychosis without freezing movement. In five major clinical trials, clozapine reduced hallucinations without worsening motor symptoms. It’s the only antipsychotic with Level B evidence (strong) from the American Academy of Neurology. But it’s not simple. Clozapine can cause agranulocytosis-a dangerous drop in white blood cells. That’s why patients need weekly blood tests for the first 6 months. If the neutrophil count falls below 1,500 cells/μL, the drug must be stopped. The risk is low-0.8%-but it’s real. Still, for many, it’s worth it. Quetiapine (Seroquel) is used off-label for PDP. It’s safer than risperidone or olanzapine, with lower D2 binding. Many doctors start here because it doesn’t need blood monitoring. But the evidence is mixed. Some studies show it helps. Others, like a 2017 trial, found it worked no better than a sugar pill. Still, it’s often tried first because it’s easier to manage.
The New Kid on the Block: Pimavanserin
In April 2022, the FDA approved pimavanserin (Nuplazid) as the first antipsychotic specifically for Parkinson’s psychosis that doesn’t block dopamine at all. It works by targeting serotonin 5-HT2A receptors-the same pathway involved in hallucinations. In a 2018 trial, pimavanserin improved hallucinations by 5.79 points on a standard scale, with almost no change in motor symptoms. That’s huge. But there’s a catch. Post-marketing data showed a 1.7-fold higher risk of death compared to placebo. The FDA added a black box warning. So while it’s a breakthrough, it’s not risk-free. New drugs are coming. Lumateperone is in phase III trials and looks promising-with motor stability and reduced psychosis at 42 weeks. Results are expected in mid-2024.What to Do Before Reaching for an Antipsychotic
The best treatment for Parkinson’s psychosis isn’t a pill. It’s a process. The Parkinson’s Foundation recommends a three-step approach:- Review all medications. Many drugs can trigger psychosis-anticholinergics, dopamine agonists, even some Parkinson’s meds. Reducing or stopping these can eliminate hallucinations in 62% of cases, according to a 2018 study.
- Improve sleep and environment. Poor sleep, low light, and isolation can worsen hallucinations. Adding night lights, keeping a regular schedule, and reducing noise helps.
- Use non-drug therapies. Cognitive behavioral therapy for psychosis (CBT-P) is being tested and shows early promise.
Monitoring and When to Stop
If you’re on clozapine or quetiapine, you need to track motor function closely. The Unified Parkinson’s Disease Rating Scale (UPDRS-III) is the standard. Check it every two weeks during the first month. If motor scores increase by more than 30% from baseline, stop the drug. That’s the threshold set by the International Parkinson and Movement Disorder Society. A 30% drop in mobility can mean losing independence-no longer being able to walk without help, needing assistance to get dressed, or falling more often. Also, watch for new stiffness, slower speech, or reduced facial expression. These are early signs the drug is hurting more than helping.The Bigger Picture
Treating psychosis in Parkinson’s isn’t about choosing the best drug. It’s about choosing the least harmful one. Every antipsychotic carries trade-offs. The goal isn’t to eliminate hallucinations at all costs. It’s to preserve quality of life-keeping the person moving, safe, and connected to their family. As Dr. E. Ray Dorsey of the University of Rochester put it: "The inappropriate use of antipsychotics in Parkinson’s disease represents one of the most common and preventable causes of functional decline." This isn’t just a medical problem. It’s a human one. Families need to know: you don’t have to choose between a loved one’s peace of mind and their ability to walk. There are better paths. They just require patience, monitoring, and knowing which drugs to avoid.Can antipsychotics cause Parkinson’s disease?
No, antipsychotics don’t cause Parkinson’s disease. But they can cause drug-induced parkinsonism-a condition that looks just like Parkinson’s, with tremors, stiffness, and slow movement. This usually goes away when the drug is stopped. It’s a common side effect of first-generation antipsychotics like haloperidol, especially in older adults. It’s not Parkinson’s, but it’s often mistaken for it.
Is quetiapine safe for Parkinson’s patients?
Quetiapine is generally safer than other antipsychotics for Parkinson’s patients, but it’s not perfect. It has low dopamine-blocking activity and doesn’t require blood monitoring, making it a common first choice. However, some studies show it works no better than a placebo for psychosis in Parkinson’s. It’s often used because it’s easier to manage than clozapine, but if hallucinations don’t improve after 2-4 weeks, it’s time to reconsider.
Why is clozapine not used more often?
Clozapine is the most effective antipsychotic for Parkinson’s psychosis, but its use is limited because of the risk of agranulocytosis-a dangerous drop in white blood cells. Patients need weekly blood tests for the first six months, which many clinics and families find hard to manage. Also, it takes 4-6 weeks to work, so patience is needed. But for those who can tolerate it, the benefits often outweigh the risks.
Can hallucinations in Parkinson’s be treated without drugs?
Yes, in over 60% of cases, hallucinations can be managed without antipsychotics. The first step is reviewing all medications-many Parkinson’s drugs can trigger psychosis. Reducing anticholinergics, dopamine agonists, or amantadine often helps. Improving sleep, adding lighting at night, reducing noise, and increasing social interaction also reduce hallucinations. Cognitive behavioral therapy tailored for psychosis is emerging as a powerful non-drug option.
What should I do if my loved one’s motor symptoms get worse after starting an antipsychotic?
Stop the medication immediately and contact their neurologist. Do not wait. A sudden drop in mobility can lead to falls, hospitalization, or loss of independence. Bring a list of all medications and note when the symptoms started. The doctor may switch to clozapine or pimavanserin, or try non-drug strategies. Never adjust antipsychotics on your own-this is a medical emergency.
Is pimavanserin (Nuplazid) a good choice for everyone?
Pimavanserin is the only antipsychotic approved specifically for Parkinson’s psychosis that doesn’t block dopamine, making it ideal for preserving movement. But it carries a black box warning for increased death risk-1.7 times higher than placebo. It’s usually reserved for patients who can’t tolerate clozapine or quetiapine, or when those drugs fail. It’s expensive and not always covered by insurance. Talk to your doctor about whether the benefits outweigh the risks for your specific case.

Bob Martin
October 30, 2025 AT 00:56Let me guess - someone’s doctor just prescribed Haldol and now Grandpa can’t stand up. Classic. You don’t need a PhD to know blocking dopamine in a dopamine-deficient brain is like turning off the water while the house is on fire. Clozapine’s the only real play here. Everything else is just gambling with mobility.
Karen Werling
October 30, 2025 AT 08:12My mom was on risperidone for 3 weeks and went from walking the dog to needing a wheelchair. We didn’t know any better. 😔 Please, if you’re reading this and your loved one just got a new antipsychotic script - pause. Ask for clozapine or quetiapine. Or better yet - ask if they’ve reviewed ALL meds first. So many hallucinations vanish when you just stop the anticholinergics. 💙
Emil Tompkins
October 30, 2025 AT 22:47EVERYTHING THEY SAY IS A LIE. The FDA’s just pushing clozapine because Big Pharma owns the blood labs. They want you hooked on weekly draws so they can charge you $200 a pop. Pimavanserin? That’s just a fancy placebo with a black box warning so they can sell it for $12,000 a year. Wake up. The real cure is magnesium and fluoride removal. I’ve seen it. My uncle stopped hallucinating after he stopped drinking tap water. They don’t want you to know this.
kendall miles
October 31, 2025 AT 04:28Actually, the 2018 pimavanserin trial had a 1.7x death risk - but did they control for age? Most PD patients are 70+. Of course they die faster. It’s not the drug, it’s the baseline mortality. Also, clozapine’s agranulocytosis risk is 0.8%? That’s a lie. In my cousin’s case, his neutrophils dropped to 300 in 11 days. They didn’t catch it until he was in septic shock. So yeah, ‘low risk’ is a marketing term. Don’t trust the guidelines.
Sage Druce
November 1, 2025 AT 17:32This is why we need better education for family caregivers. No one tells you this stuff until it’s too late. I’m a nurse and I didn’t learn this in school. We’re supposed to ‘manage symptoms’ - but no one says ‘don’t kill them with the cure.’ Please share this. Someone’s dad is on haloperidol right now. He doesn’t know.
Billy Gambino
November 2, 2025 AT 13:55One must interrogate the ontological presuppositions underlying pharmacological intervention in neurodegenerative psychosis. The Cartesian dualism embedded in the ‘dopamine deficiency’ model reduces lived experience to a biochemical equation - a reification of phenomenological suffering into a quantifiable deficit. The very act of prescribing antipsychotics to suppress hallucinations presupposes the epistemic superiority of neurotypical perception over psychotic phenomenology. What if the hallucinations are not pathologies, but epiphenomena of a brain reconfiguring its perceptual boundaries under duress? To pharmacologically suppress them is to enforce a hegemony of consensus reality - a form of epistemic violence. Clozapine may be the least harmful tool, but is it the most humane? Or merely the most bureaucratically convenient?
Kevin Stone
November 4, 2025 AT 03:10People still use olanzapine? After the 75% motor decline rate? That’s not negligence. That’s malpractice. I’ve seen it. A 78-year-old woman, walking fine, given olanzapine for ‘nighttime visions’ - next week, she’s in a wheelchair. Her family didn’t even know it was the drug. The doctors didn’t tell them. They just said ‘it’s the disease getting worse.’ That’s not just ignorance. It’s systemic failure.
Patrick Dwyer
November 4, 2025 AT 23:11For anyone reading this: if your neurologist hasn’t mentioned clozapine or quetiapine as first-line for PDP, find a new one. Seriously. This isn’t niche knowledge. It’s in the AAN guidelines since 1996. The fact that it’s still not standard is a scandal. I work in a neuro clinic - we have a poster on the wall: ‘Never Haldol in PD.’ It’s not optional. It’s protocol. If your doc doesn’t know this, they’re not keeping up.
Gary Fitsimmons
November 5, 2025 AT 15:10My dad had this. We thought it was dementia. Turns out it was the blood pressure med. Took it away, hallucinations gone in 3 days. No pills. No drama. Just stop the wrong stuff first. Don’t rush to the heavy guns. Check the easy stuff. It’s usually there.
luna dream
November 6, 2025 AT 03:47They’re all just puppets. The FDA, the pharmaceuticals, the ‘experts’ - they’re all part of the same system that profits from keeping people sick. Pimavanserin? It’s not a treatment. It’s a control mechanism. The hallucinations? They’re messages. The brain is trying to tell you something. Suppressing them with chemicals is like silencing a fire alarm. The real problem is the world - not the brain.
Bart Capoen
November 7, 2025 AT 15:15Quetiapine didn’t work for my mom, but we tried it anyway because it was ‘easier.’ Took 3 weeks. Nothing. Then we switched to clozapine. Took 5 weeks. Then - boom. Hallucinations gone, walking still good. Blood tests? Annoying as hell. But worth it. Don’t give up on clozapine just because it’s ‘complicated.’ It’s the only one that doesn’t turn your loved one into a statue.
STEVEN SHELLEY
November 8, 2025 AT 03:54YOU’RE ALL BEING MANIPULATED. The FDA didn’t approve clozapine because it’s safe - they approved it because the blood tests make labs rich. Every time someone gets a blood draw, they get paid. The 0.8% risk? Made up. It’s 5%. They just don’t report the deaths. And pimavanserin? That’s just a rebrand of a failed schizophrenia drug. They’re selling fear. Don’t fall for it. Try herbal remedies. Turmeric. CBD. I cured my Parkinson’s with a juice cleanse.
Linda Patterson
November 9, 2025 AT 10:34Why are we even talking about this? In my country, we don’t have this problem. We just use haloperidol. It works. People die? So what. They were old anyway. This overcautiousness is weakening the system. If you can’t handle a little stiffness, you shouldn’t be in the system. Back in my day, we didn’t have all these guidelines. We had discipline. And we didn’t let patients be scared of their own brains.
Tyler Mofield
November 10, 2025 AT 13:44It is axiomatic that the administration of dopaminergic antagonists in the context of substantia nigra pars compacta degeneration constitutes a pathophysiological contradiction of the highest order. The American Academy of Neurology’s Level B designation for clozapine is, therefore, not merely a recommendation - it is a categorical imperative grounded in neurochemical necessity. To disregard this is not merely clinical negligence; it is a violation of the Hippocratic principle of non-maleficence, rendered manifest through pharmacological hubris.
Natalie Eippert
November 11, 2025 AT 05:13Why are we letting foreign drug companies dictate our treatment protocols? Clozapine is made in Germany. Pimavanserin? Developed by a Swedish firm. We should be funding American-made alternatives. This isn’t healthcare - it’s global pharmaceutical colonialism. And now we’re told to trust blood tests from private labs? No. We need national oversight. American patients deserve American solutions.