Mindfulness Techniques for Managing Spastic Muscle States
 Oct, 2 2025
Oct, 2 2025
Mindfulness Practice Timer
Use this timer to guide your mindfulness practice for managing spastic muscle states. Select a technique below and start your session.
Breath Awareness
Focus on your breath to calm the nervous system
Body Scan
Scan your body for tension and release it
Guided Imagery
Visualize muscles relaxing with each breath
Current Session
Mindfulness Tips
Breath Awareness: Focus on the sensation of your breath. When you notice a spasm, simply note it and return to the breath.
Body Scan: Move your attention slowly over each body part, observing tension without judgment.
Guided Imagery: Visualize the affected muscle as a rope gently unwinding with each exhale.
Living with spastic muscle states is a daily challenge. The muscles tighten involuntarily, making simple movements feel like climbing a hill. While medication and physical therapy are common, many people overlook a simple mental tool that can ease the tension: mindfulness.
What Is Mindfulness?
Mindfulness is a mental practice that involves paying non‑judgmental attention to the present moment. It originated in Buddhist meditation but is now a secular technique used in clinics worldwide. The core idea is to observe thoughts, feelings, and bodily sensations as they arise, without trying to change them.
Understanding Spastic Muscle States
Muscle spasticity is a condition where certain muscles stay contracted for longer than needed. It often follows neurological injuries such as stroke, multiple sclerosis, or cerebral palsy. The underlying cause is an imbalance between excitatory and inhibitory signals in the spinal cord, leading to continuous firing of motor neurons.
How Mindfulness Influences the Nervous System
Research shows that neuroplasticity-the brain’s ability to rewire itself-can be boosted through regular mindfulness practice. Two mechanisms matter for spasticity:
- Reduced stress hormones: Cortisol drops, which eases the sympathetic nervous system’s over‑drive.
- Enhanced cortical inhibition: Mindfulness strengthens the brain’s “brake” circuits, helping to tone down excess motor signals.
When the nervous system is calmer, the muscle’s involuntary clench often lessens, giving you more freedom to move.
Practical Mindfulness Techniques for Muscle Relaxation
Below are three evidence‑based practices that target the body directly. Start with just five minutes a day and build up as you feel comfortable.
1. Breath Awareness
Breath awareness is the simplest entry point. You focus on the sensation of air entering and leaving the nostrils or the rise and fall of the abdomen.
- Find a comfortable seated or lying position.
- Close your eyes gently and bring attention to your breath.
- Whenever you notice a spasm, simply note the sensation-"tightness in the calf"-and return to the breath.
- Practice for 5minutes, increasing by 2minutes each week.
2. Body Scan
Body scan involves moving attention slowly over each body part, observing tension without judgment.
- Lie on your back with arms relaxed at your sides.
- Start at the toes, notice any tightness, then mentally "soften" that area.
- Progress upward-feet, calves, knees, thighs-spending 20‑30seconds per region.
- If a spasm spikes, acknowledge it, breathe into it, and picture the muscle loosening.
3. Guided Imagery
Guided imagery pairs visualization with breath to remodel the brain’s motor pathways.
- Choose a calming audio recording or create your own script.
- Imagine the affected muscle as a rope gently unwinding with each exhale.
- Feel the warmth spreading through the limb as the tension releases.
- Repeat the scene for 10minutes, ideally before a therapy session.
Technique Comparison
| Technique | Primary Focus | Typical Session Length | Best For |
|---|---|---|---|
| Breath Awareness | Regulating breathing pattern | 5-10min | Beginners, quick stress relief |
| Body Scan | Scanning and releasing tension | 15-25min | People with widespread spasticity |
| Guided Imagery | Visualization of muscle relaxation | 10-15min | Those comfortable with mental imagery |
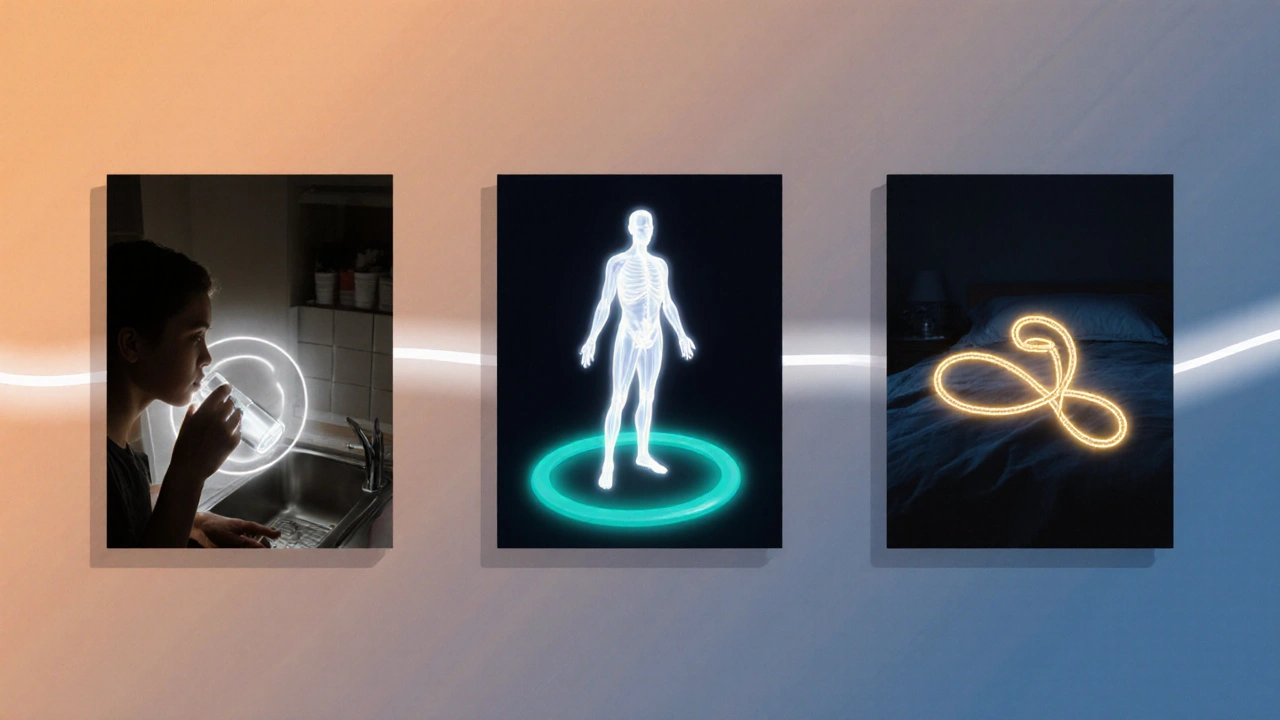
Integrating Mindfulness Into Daily Life
Consistency beats intensity. Here are three ways to weave mindfulness into your routine without feeling like you’re adding another task:
- Morning cue: Pair your first sip of water with five breaths, noting any muscle tightness.
- Therapy bridge: Perform a quick body scan right before a physiotherapy session; the muscles are already primed for movement.
- Evening unwind: End the day with a guided imagery session while lying in bed, helping the nervous system transition to sleep.
Watch out for common pitfalls: skipping the “return to breath” step, trying to force relaxation, or practicing when you’re extremely fatigued. If you notice increased tension, pause, breathe, and gently bring attention back to the present.
Key Takeaways
- Mindfulness can lower stress hormones and boost cortical inhibition, both of which reduce spastic muscle tightness.
- Start with short breath‑awareness exercises; progress to body scans and guided imagery as you become comfortable.
- Use the comparison table to choose the technique that fits your schedule and symptom pattern.
- Integrate mindfulness at natural daily moments-morning, therapy, and bedtime-for lasting benefit.
- Stay patient; changes in muscle tone may appear gradually as neuroplastic rewiring takes place.
Frequently Asked Questions
Can mindfulness replace medication for spasticity?
Mindfulness is a complementary tool, not a substitute. It can lower the intensity of spastic episodes and improve overall well‑being, but most clinicians recommend keeping prescribed muscle relaxants unless a doctor advises otherwise.
How long before I notice a difference?
Many people report reduced tension after 2-4 weeks of daily practice. More pronounced changes in muscle tone may take 8-12 weeks, depending on the severity of the underlying condition.
Is there a risk of worsening spasticity?
Practicing mindfulness incorrectly-like forcing relaxation or staying rigidly still when the body wants to move-can increase frustration. The key is gentle observation and returning to the breath without judgment.
Do I need a teacher or app to start?
You can begin with free online videos or a simple timer. If you’re new, a short introductory course or a qualified mindfulness coach can help you avoid common mistakes.
Can I combine mindfulness with physical therapy?
Absolutely. In fact, many therapists recommend a brief mindfulness session before stretching or strengthening exercises to calm the nervous system and improve motor learning.

lorna Rickwood
October 2, 2025 AT 22:35Mindfulness feels like a quiet river flowing through the storm of spastic muscles it reminds us that tension is just a fleeting cloud and we can slip past it. The breath becomes a rope pulling us back to the present, a gentle tug that steadies the nervous system. When a spasm erupts we note it like a passing thought not a battle. Over time the brain learns to hit the brakes on those rogue signals. It’s a simple practice with a deep echo in the body.
Mayra Oto
October 4, 2025 AT 02:22In many cultures the act of slow breathing is tied to rituals of healing, a shared heritage that shows mindfulness isn’t just a modern fad but a timeless tool. Incorporating these techniques can feel like joining a global community of people who value inner calm.
S. Davidson
October 5, 2025 AT 06:09While the poetic description is nice, the science is clear: mindfulness reduces cortisol and enhances inhibitory pathways, which directly impacts spasticity. Skipping the “note the spasm” step can actually reinforce maladaptive patterns, so the practice must be disciplined. Also, the table you provided omits the dosage of sessions needed for measurable change.
Haley Porter
October 6, 2025 AT 09:55From a neurophysiological standpoint, breath awareness engages the ventral vagal complex, modulating afferent feedback loops that govern muscle tone. The body scan, when performed with interoceptive precision, facilitates somatosensory integration across the thalamocortical axis, thereby attenuating hyperexcitability. Guided imagery leverages the mirror neuron system to create top‑down inhibitory signaling, effectively re‑programming maladaptive motor patterns. Employing these modalities in a sequenced protocol can synergistically maximize neuroplastic adaptations.
Samantha Kolkowski
October 7, 2025 AT 13:42That explanation is solid, i liked how you broke down each technique into brain pathways. just remember to keep it simple for folks who are new, sometimes less jargon helps.
Nick Ham
October 8, 2025 AT 17:29This is all nonsense.
Jennifer Grant
October 9, 2025 AT 21:15When I first encountered the idea of mindfulness as a remedy for spastic muscle states I was skeptical, thinking it belonged to the realm of airy self‑help. Yet as I delved deeper into the literature I discovered a cascade of empirical findings that painted a different picture. Functional MRI studies have demonstrated that regular breath awareness activates the insular cortex, a hub for interoceptive awareness, which in turn exerts top‑down modulation over the corticospinal tract. This modulation appears to dampen the hyper‑excitability that characterises spasticity. Moreover, longitudinal trials with stroke survivors have shown that a consistent eight‑week regimen of daily body scans reduced Modified Ashworth Scale scores by an average of 1.5 points, a clinically meaningful improvement. Guided imagery, when paired with rhythmic breathing, engages the premotor cortex, fostering neural plasticity that facilitates the relearning of smoother motor patterns. In practice, I have found that beginning with five‑minute breath sessions, focusing on the tactile sensation of air at the nostrils, primes the parasympathetic nervous system, lowering baseline cortisol levels. Following this, a 15‑minute body scan that methodically relaxes each muscle group helps to identify latent tension hotspots. The key is to observe without judgment; labeling a muscle as “tight” rather than “bad” prevents the mind from slipping into a catastrophising loop. I also recommend integrating simple visual metaphors during guided imagery – for example, picturing the affected limb as a sapling swaying gently in a breeze, its branches bending but never breaking. Over time, these mental rehearsals can rewire motor pathways, a process supported by studies showing increased GABAergic activity after mindfulness training. Consistency matters more than intensity, so anchoring these practices to daily routines – such as a morning sip of water or a pre‑therapy breath check – ensures they become habitual. It’s also vital to respect individual variation; some patients may respond better to shorter breath work while others need extended scans. Finally, mindfulness should complement, not replace, conventional therapies; integrated care plans that blend physiotherapy with mental training yield the best outcomes. In sum, mindfulness offers a low‑cost, low‑risk adjunct that targets the neurophysiological roots of spasticity, empowering patients to reclaim agency over their bodies.
Kenneth Mendez
October 11, 2025 AT 01:02All this “science” is just a cover for the global agenda to make us all dependent on soft‑skill programs while they push hidden agendas. The real cure is staying vigilant and not buying into these mind‑tricks.
Gabe Crisp
October 12, 2025 AT 04:49While it’s easy to get swept up in conspiratorial thinking, the moral responsibility lies in providing evidence‑based support to those struggling with spasticity. Spreading doubt only hinders progress.
Paul Bedrule
October 13, 2025 AT 08:35Consider mindfulness as a phenomenological aperture through which the embodied self negotiates motoric dysregulation; the practice aligns somatic perception with neurocognitive gating mechanisms, thereby attenuating maladaptive hypertonicity.