Antipsychotic Side Effects: Metabolic Risks and How to Monitor Them
 Nov, 17 2025
Nov, 17 2025
When you start taking an antipsychotic, the goal is clear: reduce hallucinations, calm delusions, and bring back some stability. But for many people, the relief comes with a hidden cost-weight gain, high blood sugar, and rising cholesterol. These aren’t just inconvenient side effects. They’re life-threatening risks that can shorten your life by decades. The truth is, if you’re on a second-generation antipsychotic like olanzapine or clozapine, your body is under metabolic stress. And if no one is checking your blood pressure, waist size, or fasting glucose, you’re flying blind.
Why Metabolic Risks Are Not Just a Side Note
Second-generation antipsychotics (SGAs) were meant to be safer than older drugs. They cut down on tremors and stiffness, which was a big win. But in the 2000s, the hidden price started showing up in hospital records and autopsy reports. People on these medications were dying younger-not from suicide or accidents, but from heart attacks and strokes. The reason? Metabolic syndrome. It’s not one thing. It’s a cluster: belly fat, high triglycerides, low good cholesterol, high blood pressure, and high blood sugar. And it’s happening to 32% to 68% of people taking SGAs, compared to just 3% to 26% of people not on these drugs.Which Antipsychotics Carry the Highest Risk?
Not all antipsychotics are created equal when it comes to metabolism. Some are like slow-burning fires; others are explosions.- Olanzapine and clozapine are the worst offenders. In the CATIE study, people gained an average of 2 pounds per month during the first 18 months. About 30% gained over 7% of their body weight. Blood sugar spikes happen even without weight gain-these drugs directly mess with insulin.
- Quetiapine and risperidone are in the middle. Weight gain is common, but less extreme. Blood sugar issues are real, especially with long-term use.
- Aripiprazole, ziprasidone, and lurasidone are the safest. Weight gain is minimal-often less than 5% of patients gain significant weight. Blood sugar and cholesterol stay closer to normal.
Why the difference? It’s about receptors in the brain. Drugs that block histamine H1 and serotonin 5-HT2C receptors are the ones that make you hungry and mess with how your body handles sugar. Olanzapine hits both hard. Aripiprazole barely touches them.
What Gets Monitored-and When
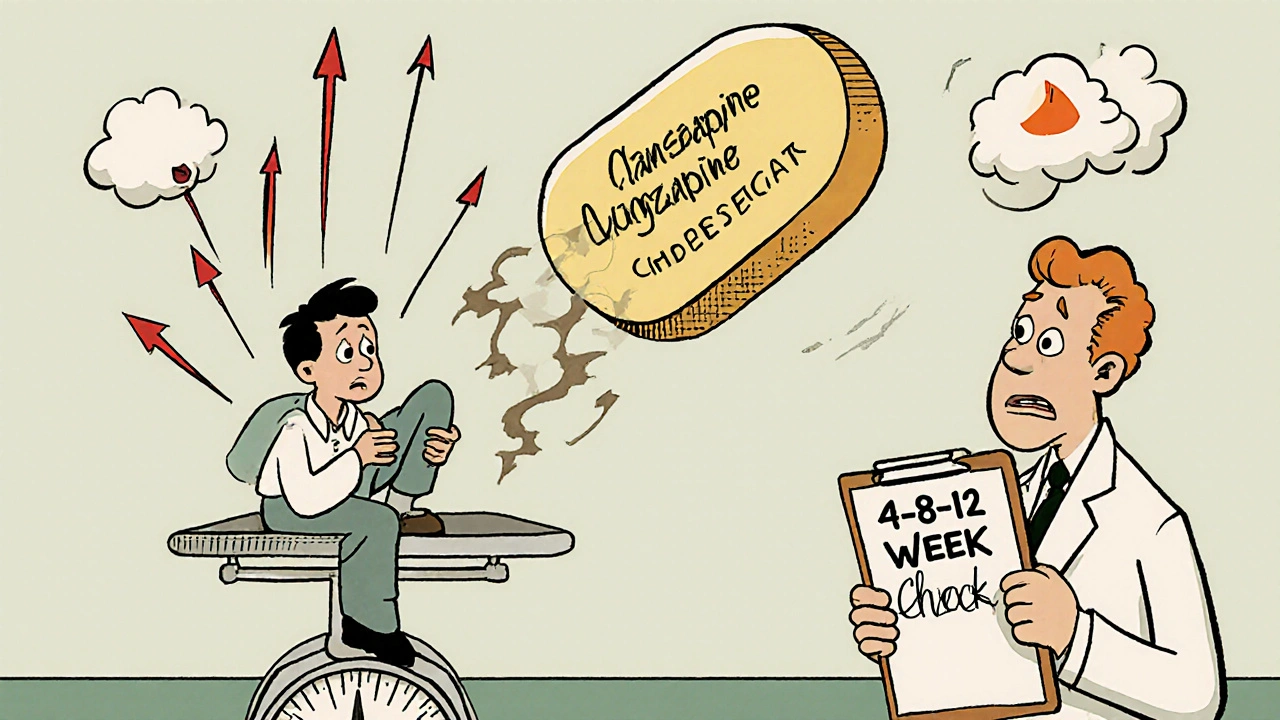
Guidelines from the American Psychiatric Association and the American Diabetes Association are clear: you need baseline checks before starting, then regular follow-ups. But in practice? Too many people never get tested.Here’s what should happen:
- Before starting: Weight, waist circumference, blood pressure, fasting blood sugar, and lipid panel (cholesterol and triglycerides).
- At 4, 8, and 12 weeks: Repeat all the above. This is when most weight gain and blood sugar changes happen.
- Every 3 months for the first year: Keep tracking. If things start moving up, you need to act.
- Annually after that: Minimum. If you’re on high-risk meds like olanzapine, quarterly checks are better.
Waist size matters more than weight. A waist over 40 inches in men or 35 inches in women signals dangerous fat around your organs-even if your BMI looks okay.
What Happens If You Ignore It?
People don’t realize how fast this can go wrong. One patient on Reddit shared gaining 45 pounds in six months on olanzapine. By year two, he had prediabetes. He switched to aripiprazole-and lost 30 pounds in nine months. His blood sugar returned to normal.But not everyone can switch. Clozapine is the most effective drug for treatment-resistant schizophrenia. It cuts death risk by half compared to other antipsychotics. So the choice isn’t simple: better mental control vs. worse physical health.
Studies show that patients on high-risk antipsychotics have a 3-fold higher risk of developing type 2 diabetes and cardiovascular disease than those not on them. And because psychiatric patients already have higher rates of smoking, poor diet, and inactivity, the risk stacks up. The result? A 20- to 25-year gap in life expectancy compared to the general population.
Why Doctors Don’t Always Monitor
It’s not that they don’t care. It’s that the system isn’t built for this.- Psychiatrists aren’t trained in metabolic care. They’re focused on mood, thoughts, and behavior.
- Primary care doctors don’t always know a patient is on antipsychotics.
- Patients avoid blood tests because they’re afraid of bad news-or they’ve been told to “just lose weight” without support.
- Electronic health records rarely have built-in alerts for antipsychotic monitoring.
A 2022 survey found only 38% of U.S. psychiatrists consistently follow the recommended monitoring schedule. In New Zealand, Australia, and the UK, it’s often worse in public clinics due to time and resource limits.
What Can You Do?
You’re not powerless. Here’s how to take control:- Ask for your baseline results. Don’t wait for your doctor to bring it up. Request weight, waist, blood pressure, fasting glucose, and lipids before your first dose.
- Track your own numbers. Keep a notebook or use a free app. Note any changes in appetite, energy, or thirst.
- Push for early intervention. If you gain more than 5% of your body weight in 3 months, ask about switching meds or adding lifestyle support. Don’t wait until you’re diabetic.
- Find a team. Look for clinics with integrated care-where a psychiatrist, dietitian, and nurse work together. Kaiser Permanente and Massachusetts General Hospital have shown this cuts weight gain by 50%.
- Consider alternatives. If you’re on olanzapine or clozapine and doing okay, ask: “Is there a lower-risk option that still works for me?” Aripiprazole or lurasidone might be worth a trial.
The Future Is Changing
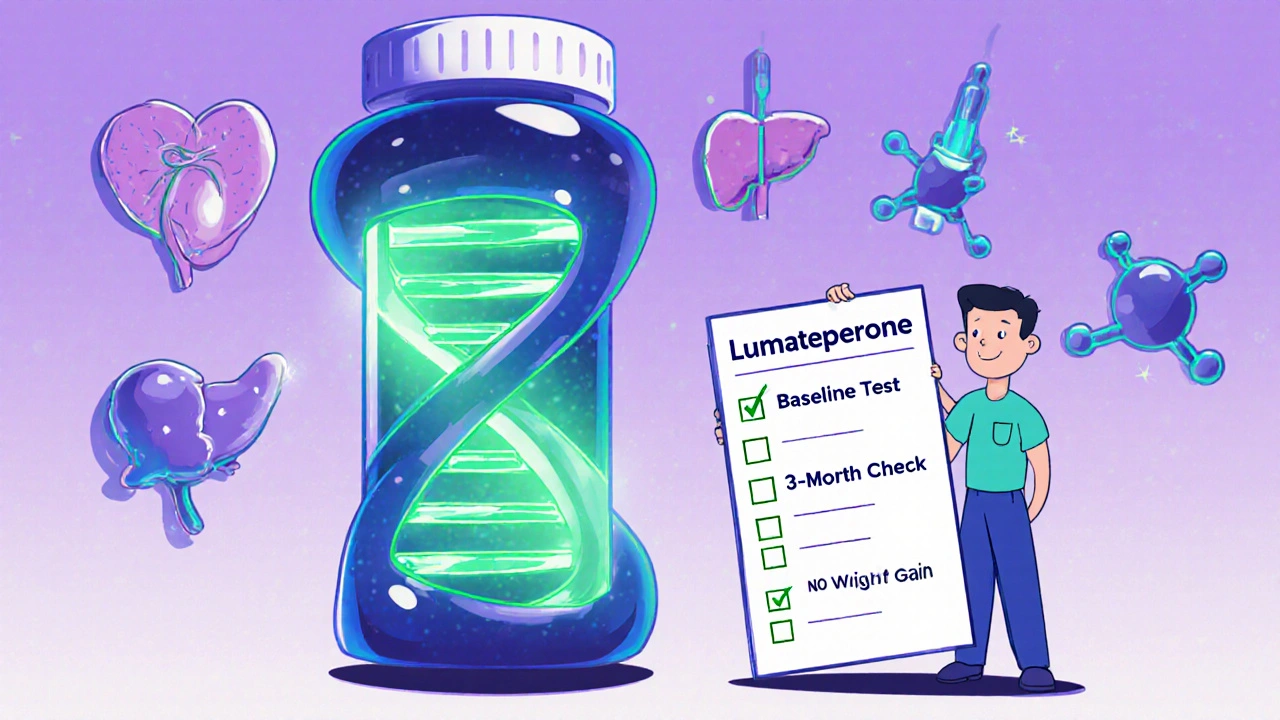
Good news: the tide is turning. In 2023, the FDA approved lumateperone (Caplyta), a new antipsychotic with minimal metabolic impact-only 3.5% of users gained weight, compared to 23.7% on olanzapine. It’s not a miracle drug, but it’s proof that better options are possible.The National Institute of Mental Health is funding a $12.5 million study to predict who’s genetically at risk for metabolic side effects. By 2025, we might be able to test your DNA before prescribing-and pick the drug that’s safest for your body.
For now, the message is simple: don’t assume your mental health provider is watching your physical health. You have to be the advocate. Ask for the tests. Track your numbers. Push for change. Because your life isn’t just about quieting voices-it’s about living long enough to enjoy the peace they bring.
Do all antipsychotics cause weight gain?
No. Weight gain varies widely by medication. Olanzapine and clozapine cause the most-up to 30% of users gain 7% or more of their body weight. Aripiprazole, ziprasidone, and lurasidone have the lowest risk, with weight gain in fewer than 5% of users. The difference comes from how each drug interacts with brain receptors that control hunger and metabolism.
Can I avoid metabolic side effects just by eating better and exercising?
Lifestyle changes help-but they rarely fully offset the biological impact of high-risk antipsychotics. Studies show that even with diet and exercise, people on olanzapine or clozapine still gain weight and develop insulin resistance. The drugs directly interfere with how your body processes sugar and fat. That’s why medication choice matters as much as behavior.
How often should I get my blood sugar checked?
Before starting the medication, get a fasting glucose test. Then check again at 4, 8, and 12 weeks. If results are normal, check every 3 months for the first year. After that, at least once a year. If you’re on a high-risk drug like olanzapine, or if your numbers start rising, check every 3 months indefinitely.
What if my doctor says the benefits outweigh the risks?
That’s often true-for clozapine in treatment-resistant schizophrenia, the benefits are life-saving. But that doesn’t mean you shouldn’t monitor. Even if you stay on a high-risk drug, regular checks let you catch problems early. You can still manage blood pressure, cholesterol, and blood sugar with medication or lifestyle changes. The goal isn’t to stop treatment-it’s to protect your body while keeping your mind stable.
Are there new antipsychotics with fewer side effects?
Yes. Lumateperone (Caplyta), approved in 2023, causes minimal weight gain and has no significant impact on blood sugar or cholesterol. Other newer drugs like asenapine and iloperidone also have better profiles than older SGAs. While they’re not perfect, they offer real alternatives-especially if you’re on olanzapine or clozapine and struggling with weight or blood sugar.
Why don’t more doctors monitor for metabolic risks?
Many psychiatrists aren’t trained in metabolic health, and primary care doctors often don’t know their patients are on antipsychotics. Time is limited in appointments, and electronic records rarely have automated alerts for these checks. In public health systems, resources are stretched thin. It’s not negligence-it’s a system failure. That’s why patients need to speak up and ask for testing.

kora ortiz
November 17, 2025 AT 13:57You don't have to accept this as inevitable. I was on olanzapine for 18 months and gained 50 pounds. Switched to aripiprazole. Lost 40 in 8 months. My glucose is normal now. It's not magic. It's just knowing your options. Ask for the tests. Demand the follow-ups. Your body deserves more than a footnote in a psychiatric chart.
Jeremy Hernandez
November 18, 2025 AT 04:07Lol so now we're supposed to trust Big Pharma's new 'safe' antipsychotics? Lumateperone? That's just the same poison in a prettier bottle. They don't care if you live or die as long as you keep buying pills. The real fix? Get off all meds. Go primal. Eat meat. Sleep in the dark. Stop listening to doctors who think a blood test is a 'recommendation' and not a goddamn lifeline.
Tarryne Rolle
November 19, 2025 AT 07:42It's ironic isn't it? We're told to 'manage' our minds with chemicals, yet our bodies are treated like collateral damage. The real tragedy isn't the weight gain or the diabetes-it's that we've normalized this. We've accepted that mental health means trading your longevity for silence. But silence isn't peace. It's surrender. And surrender isn't recovery-it's just a slower kind of death dressed in white coats.
Kyle Swatt
November 20, 2025 AT 22:19Man I’ve been on this ride. Clozapine saved my life from the voices but nearly killed me with insulin resistance. I didn’t know my waist was a ticking bomb until I hit 42 inches. Then I started walking 2 miles a day. Not because I was told to. Because I refused to let a drug decide how long I’d live. It ain’t pretty. It ain’t easy. But you’re not a patient. You’re a person with a pulse. And pulses don’t get silenced by prescriptions.
Deb McLachlin
November 21, 2025 AT 12:02While the information presented is largely accurate and well-referenced, it is important to note that metabolic monitoring protocols vary significantly across international healthcare systems. In Canada, for instance, provincial guidelines often mandate quarterly metabolic screening for patients on second-generation antipsychotics, with electronic alerts integrated into primary care systems. This structural support significantly improves adherence. The disparity in care delivery between private and public systems remains a critical equity issue.
saurabh lamba
November 21, 2025 AT 15:10lol why even take meds if they turn you into a fat diabetic? just meditate and talk to your ghosts. they’re probably just lonely. also i heard the government puts stuff in the water to make you fat so you need more pills. 🤔
Kiran Mandavkar
November 21, 2025 AT 20:47Anyone who thinks lifestyle changes can offset olanzapine’s metabolic havoc is delusional. This isn’t about willpower-it’s about pharmacology. Your insulin receptors are hijacked. Your adipocytes are reprogrammed. You think eating kale fixes that? Please. The only ethical choice is to prescribe the lowest-risk agent from day one. If your doctor doesn’t know this, they’re not a doctor-they’re a liability.
Eric Healy
November 23, 2025 AT 06:50They never tell you the real reason they push olanzapine-its cheap. Insurance loves it. Docs love it. Patients? They just want the voices to stop. So we let them get fat and diabetic. And then we blame them for not exercising. Real compassionate care right here.
Shannon Hale
November 25, 2025 AT 05:55MY BROTHER DIED AT 38 FROM A HEART ATTACK ON CLOZAPINE. NO ONE CHECKED HIS CHOLESTEROL. NO ONE ASKED ABOUT HIS WAIST. THEY JUST SAID 'HE WASN'T FOLLOWING INSTRUCTIONS.' WHAT INSTRUCTIONS? THE ONES WRITTEN IN A BROCHURE HE COULDN'T READ BECAUSE HIS BRAIN WAS FRIED? I'M SO ANGRY I CAN'T BREATHE. THIS IS MURDER BY INDIFFERENCE.
Holli Yancey
November 25, 2025 AT 14:26I just want to say thank you to everyone who’s shared their story here. I’m on risperidone and I’ve been terrified to bring up weight gain. But reading this… I think I’ll ask for my labs next week. Maybe I don’t have to choose between peace and a body that works. Maybe I can have both if I speak up.
kora ortiz
November 25, 2025 AT 21:49That’s the spirit. One test at a time. One conversation with your doctor. One refusal to be silent. You’re not asking for a favor-you’re claiming your right to live. And that’s not weakness. That’s the bravest thing you’ll ever do.