Why Generic Combination Products Improve Patient Compliance
 Feb, 16 2026
Feb, 16 2026
When patients have to take multiple pills every day, they often forget, skip doses, or stop altogether. It’s not laziness - it’s human. A study found that adherence drops by 26% when a daily routine goes from once-daily to twice-daily dosing. That’s why doctors and pharmacists are turning to combination products: single units that deliver two or more medications in one package. And when those are generic, the benefits stack up even higher - not just in cost, but in real-world adherence.
What Exactly Are Generic Combination Products?
A combination product isn’t just two pills in one bottle. It’s a single unit that merges a drug with a delivery device. Think insulin pens, inhalers, auto-injectors, or even patches that release medicine slowly through the skin. These aren’t new - insulin pens have been around for decades, and drug-eluting stents have saved thousands of hearts. But what makes them powerful is how they simplify treatment.Generic versions of these products copy the original brand-name combination product exactly - same active ingredients, same delivery mechanism, same dose accuracy. The FDA requires them to match the brand in performance: whether it’s the force needed to activate an auto-injector (5-15 Newtons), the precision of a dose (within ±5%), or how consistently a patch releases medication over hours. If it doesn’t perform the same, it doesn’t get approved.
Unlike simple generic pills, generic combination products must pass two sets of tests - one for the drug, one for the device. That’s why they take longer to hit the market - 18 to 24 months longer than a regular generic drug. But once they do, they bring huge advantages.
The Compliance Edge: One Unit, Not Five
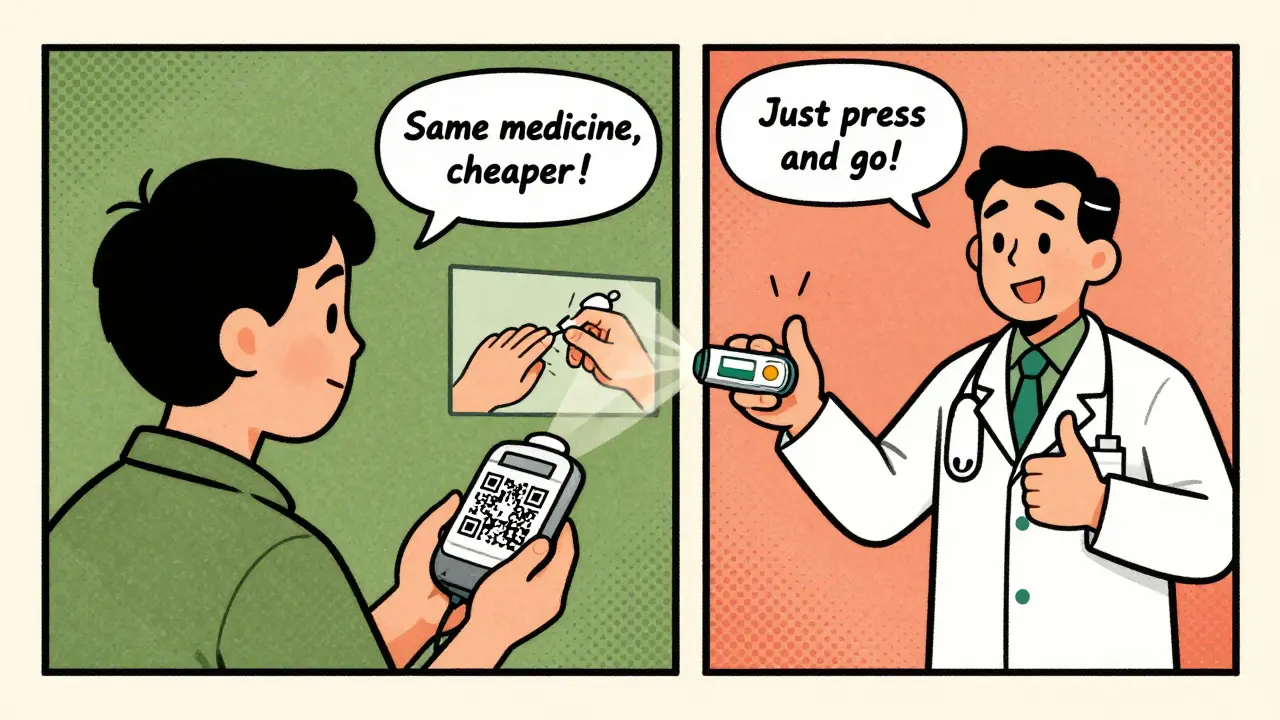
Imagine you’re managing diabetes, high blood pressure, and high cholesterol. That’s three different pills, maybe taken at different times of day. Now imagine a single pill that combines two of those drugs, and an auto-injector for the third. Suddenly, your daily routine is simpler. Fewer pills. Fewer bottles. Fewer chances to mess up.Studies show combination products improve adherence by 15% to 25% compared to taking separate medications. Why? Because complexity kills compliance. A survey of patients using combination products found that 78% said the ease of use made them more likely to stick with their treatment.
Real stories back this up. On Reddit’s r/Diabetes forum, users shared how switching from vials and syringes to prefilled insulin pens cut their dosing errors from 3-4 per week to nearly zero. No more measuring, no more fumbling with needles. Just press and go. That’s not a minor convenience - it’s life-changing for someone managing a chronic condition.
Why Generic Versions Work Better Than Brand-Name
Brand-name combination products are expensive. A single insulin pen can cost over $100 without insurance. That price tag is why 23.4% of patients skip doses because they can’t afford them.Generic versions cost 30% to 80% less. And here’s the key: they don’t sacrifice effectiveness. A study found that patients who started on generic medications were 8.7 percentage points more likely to stick with their regimen than those who started on brand-name drugs. Why? Because cost is a huge barrier - remove it, and adherence climbs.
But it’s not just about price. Generic combination products also preserve the design features that make the original so effective. A generic inhaler must deliver the same amount of medicine with the same puff technique. A generic auto-injector must click the same way, feel the same, and work the same. If it doesn’t, patients get confused - and stop using it.

The Hidden Challenge: Switching Between Generics
Here’s where things get tricky. Unlike a generic pill, where all versions look and work the same, generic combination products can have different devices. Two different generic versions of the same inhaler might have slightly different mouthpieces, button placements, or inhalation instructions.One patient might get Generic A this month. Next month, their pharmacy fills it with Generic B. They don’t realize the device changed. They use it the same way - and miss their dose. On PatientsLikeMe, a COPD patient wrote: “Each generic version required slightly different breathing techniques. I missed doses until I got trained again.”
This isn’t rare. Avalere Health found that inconsistent substitution practices affected 32% of patients using combination products. It’s not the fault of the generics - it’s the lack of consistency across manufacturers. The FDA is working on new guidance to fix this, but right now, it’s a gap in the system.
How to Maximize Compliance With Generic Combination Products
The good news? The biggest barrier isn’t the product - it’s the handoff. Here’s what works:- Train patients properly. A 10-minute demo on how to use a generic auto-injector or inhaler can boost adherence by 17% to 22%. Don’t assume they know how it works.
- Explain why the pill looks different. Many patients think a change in color or shape means it’s weaker. Tell them: “Same active ingredient. Same dose. Just cheaper.”
- Use visual aids. Clear diagrams, QR codes linking to video tutorials, or even simple stickers on the packaging help. Biobuzz found that injection systems and inhalers with clear instructions had 40% higher adherence.
- Stick to one generic version. If possible, ask the pharmacy to keep filling the same generic. Consistency matters more than cost savings if it means fewer mistakes.
Doctors and pharmacists who take 2-3 minutes to walk patients through their new combination product see better outcomes. It’s not just about prescribing - it’s about coaching.
The Bigger Picture: Why This Matters Now
The global market for combination products hit $127.5 billion in 2022 and is expected to grow to $258.3 billion by 2030. Diabetes alone accounts for 28% of that market - mostly through insulin pens and delivery systems.The Inflation Reduction Act of 2022 is pushing more generic competition. By 2026, generic combination product approvals are expected to jump by 40%. More options mean more access - but only if patients can use them safely.
Physicians are already on board. 62% of doctors prefer combination products for chronic disease management because they see the adherence gains firsthand. The question isn’t whether these products work - it’s whether we’re doing enough to help patients use them right.
Bottom Line: Simplicity + Affordability = Better Health
Generic combination products aren’t just cheaper versions of brand-name drugs. They’re smarter, simpler tools that remove two of the biggest reasons people stop taking their medicine: complexity and cost.When done right, they reduce pill burden, cut errors, and make treatment feel less like a chore. But they only work if patients understand how to use them - and if pharmacies don’t keep switching them out without warning.
The future of chronic disease management isn’t more pills. It’s fewer, smarter, and more affordable ones. Generic combination products are leading that shift. The question now is: are we ready to support the people who depend on them?
Are generic combination products as effective as brand-name ones?
Yes. The FDA requires generic combination products to match the brand-name version in every way that matters: same active ingredients, same dose accuracy, same device performance. Whether it’s an auto-injector, inhaler, or patch, the generic must deliver the same results. Studies confirm that patients achieve the same clinical outcomes with generics as with brand-name versions.
Why do some patients have trouble with generic combination products?
The main issue is inconsistent device design between different generic versions. Two generics of the same inhaler might have different mouthpieces, button placements, or activation methods. If a patient switches between them without proper retraining, they may use it incorrectly and miss doses. This isn’t a flaw in the generics themselves - it’s a gap in how pharmacies substitute them.
Do generic combination products cost less?
Yes, significantly. Generic combination products typically cost 30% to 80% less than their brand-name equivalents. For chronic conditions like diabetes or asthma, where patients need these products long-term, that savings can mean the difference between consistent use and skipping doses due to cost.
Can pharmacists substitute one generic combination product for another?
Legally, yes - but it’s not always safe. Unlike generic pills, where all versions are nearly identical, combination products involve devices that can vary slightly between manufacturers. If a patient is switched from one generic inhaler to another without counseling, they may use it wrong. Many experts recommend sticking with one generic version unless the patient is properly retrained.
How can I ensure I’m using my generic combination product correctly?
Ask your pharmacist or doctor for a quick demonstration. Don’t assume you know how it works just because you used the brand-name version. Check the packaging for diagrams or QR codes that link to instructional videos. If the device looks different, speak up - and don’t hesitate to request the same generic version each time. Consistency helps prevent mistakes.

Agnes Miller
February 16, 2026 AT 20:47Pharmacist even gave him a little sticker with a QR code to a 30-second video. That helped more than the pamphlet.