Statin Intolerance Clinics: How Structured Protocols Help Patients Tolerate Cholesterol Medication
 Dec, 27 2025
Dec, 27 2025
Statin Tolerance Calculator
Your Personalized Statin Tolerance Assessment
This calculator helps determine your potential to tolerate statins based on clinical evidence from top lipid clinics. Results reflect real-world outcomes from studies like Cleveland Clinic and Kaiser Permanente.
Your Treatment Pathway
LDL Reduction Potential
Recommended Approach
Millions of people take statins to lower their cholesterol and reduce their risk of heart attacks and strokes. But for some, the side effects - especially muscle pain, weakness, or cramps - are too much to handle. Many patients are told to stop statins altogether, leaving them vulnerable to cardiovascular events. That’s where statin intolerance clinics come in. These specialized programs don’t just say ‘stop the drug.’ They find a way to keep you protected - without the pain.
What Is Statin Intolerance, Really?
Statin intolerance isn’t just feeling sore after a workout. It’s when muscle symptoms start within 2 to 4 weeks of taking a statin and go away 2 to 4 weeks after stopping it. The key is timing and pattern. The National Lipid Association (NLA) updated its definition in 2022: statin intolerance is a spectrum of symptoms linked to statin use, not just one fixed reaction. It’s not about lab numbers alone - though high CK levels (above 10 times the normal limit) can help confirm it. But many patients have muscle pain with normal CK. That’s why clinics focus on symptoms first, labs second.Here’s the catch: up to 80% of people who think they’re statin intolerant might actually tolerate statins - if tested properly. A blinded rechallenge (where neither patient nor doctor knows if it’s the real drug or placebo) often reveals that the pain was psychological, not physical. But most doctors skip this step. That’s why specialized clinics are changing the game.
How Statin Intolerance Clinics Work
These clinics follow a clear, step-by-step protocol - not guesswork. The standard process starts with stopping the statin completely for at least two weeks. During that time, patients track their symptoms daily: where the pain is, how bad it is (on a 0-10 scale), and whether it improves. If the pain fades, it’s a strong sign the statin was the cause.Next, they rule out other causes. Low thyroid function? Low vitamin D? Drinking too much alcohol? Taking supplements like red yeast rice? These can all mimic statin side effects. A simple blood test for TSH, vitamin D, and creatine kinase (CK) can clear up confusion. At Kaiser Permanente and Cleveland Clinic, skipping this step leads to misdiagnosis in nearly 40% of cases.
Then comes the rechallenge - the most important part. Instead of trying the same statin again, clinics switch to a different one. Lipophilic statins like simvastatin and atorvastatin soak into muscle tissue easily. Hydrophilic statins like pravastatin and rosuvastatin are designed to target the liver. Switching from simvastatin to rosuvastatin works for about 72% of patients who thought they couldn’t tolerate any statin.
What If You Still Can’t Tolerate Statins?
If switching statins doesn’t work, clinics don’t give up. They use proven alternatives - carefully chosen and monitored.- Ezetimibe is the first-line option. It blocks cholesterol absorption in the gut. It reduces LDL by about 15-20%, costs around $35 a month, and has been shown in the IMPROVE-IT trial to cut major heart events by 6% over 7 years.
- Bempedoic acid (Nexletol) works in the liver like a statin but doesn’t enter muscle cells. It lowers LDL by 18-20% and causes almost no muscle pain. It’s more expensive - about $491 a month - but many insurers cover it after statin failure.
- PCSK9 inhibitors (evolocumab, alirocumab) are injectables that slash LDL by 50-60%. But they cost $5,850 a year. Insurance often denies them unless you’ve tried at least two statins and ezetimibe. Some clinics help patients appeal these denials - and win 60% of the time.
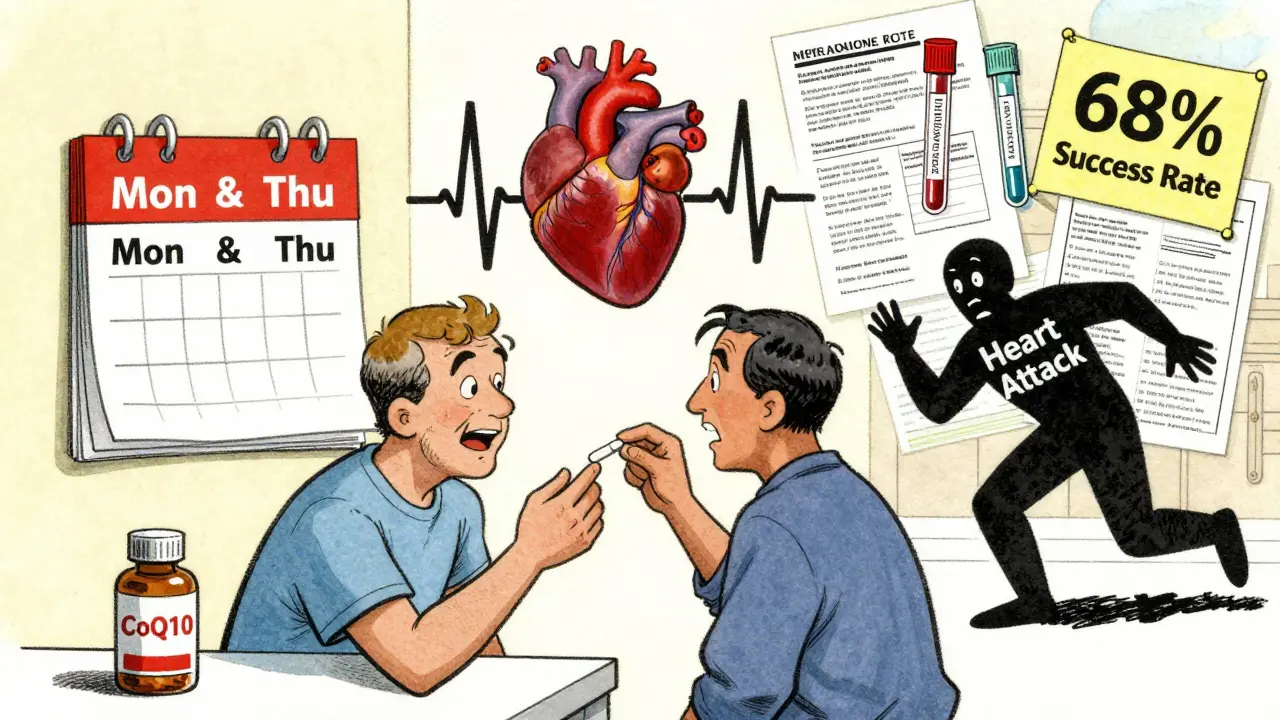
Intermittent dosing is another powerful tool. Instead of daily statins, patients take rosuvastatin or atorvastatin just twice a week. A Cleveland Clinic study of 1,247 patients found 76% tolerated this approach and still lowered LDL by 20-40%. It’s not FDA-approved for this use, but it’s backed by real-world data and used in top lipid centers.
Why Most Doctors Miss This
Primary care doctors aren’t trained to manage statin intolerance systematically. They see a patient with muscle pain, say ‘stop the statin,’ and move on. But that leaves patients at risk. A 2017 study in the Journal of Managed Care & Pharmacy showed that without a structured approach, 45% of patients permanently stop statins. In clinics with protocols, that number drops to 18%.Also, many doctors don’t know how to use the ACC’s Statin Intolerance Tool, launched in March 2023. This free online tool helps clinicians calculate a patient’s risk of heart disease versus the risk of side effects. It suggests alternatives based on age, cholesterol levels, diabetes status, and family history. It’s not magic - but it’s the closest thing to a roadmap.
What Patients Are Saying
On Reddit, a user named HeartPatient87 wrote: ‘After being labeled statin intolerant for 5 years, the lipid clinic at Johns Hopkins had me on rosuvastatin 5mg twice weekly with CoQ10 - LDL dropped from 142 to 89 without muscle pain.’Kaiser Permanente’s internal survey in 2022 found that 82% of patients in their statin intolerance program were able to restart lipid-lowering therapy. Compare that to 45% in regular care. The most common praise? The structured rechallenge process and personalized dosing.
But there are frustrations. Wait times for specialist appointments can be 6 to 8 weeks. Insurance often denies coverage for newer drugs like bempedoic acid or PCSK9 inhibitors, even when guidelines say they’re appropriate. One patient on Inspire’s forum spent 11 weeks and four appeals to get PCSK9 coverage - and still had to pay $200 a month out of pocket.
The Bigger Picture
Cardiovascular disease is still the #1 cause of death worldwide. Statins reduce major events by 20-25% for every 1 mmol/L drop in LDL. That’s massive. But if patients stop because of side effects, that benefit disappears.Statin intolerance clinics are filling a gap that’s been ignored for too long. They don’t just manage side effects - they restore confidence. They turn patients from ‘I can’t take statins’ to ‘I found a way to stay protected.’
As of 2024, 63 of the 100 largest U.S. health systems have formal statin intolerance protocols. Academic centers lead the way - 87% have them. Community hospitals? Only 42%. That gap needs to close.
Emerging tools are making this even better. Mayo Clinic now tests for the SLCO1B1 gene variant, which increases risk of simvastatin muscle damage. If you have it, avoid simvastatin - no rechallenge needed. Nanoparticle statins, still in trials, show 92% tolerability in early results. These aren’t science fiction - they’re the next step.
What You Can Do Today
If you’ve been told you’re statin intolerant:- Don’t assume it’s permanent. Ask for a referral to a lipid specialist or statin intolerance clinic.
- Request a CK test and thyroid/vitamin D check before giving up.
- Ask if switching to rosuvastatin or pravastatin is an option.
- Ask about twice-weekly dosing - it’s safe and effective for many.
- If alternatives are denied, ask for help appealing insurance.
You don’t have to choose between heart health and muscle pain. There’s a middle path. It just takes the right system to find it.
Can you really be statin intolerant if your CK levels are normal?
Yes. Many patients have muscle pain with normal CK levels. The 2022 NLA guidelines say clinical symptoms matter more than lab numbers. If pain starts after starting a statin and goes away after stopping it, that’s enough to suspect intolerance - even if CK is normal. Labs support the diagnosis, but they don’t define it.
Is ezetimibe as good as a statin for preventing heart attacks?
It’s not as strong, but it’s proven. The IMPROVE-IT trial showed ezetimibe added to a statin reduced heart attacks and strokes by 6% over 7 years. For people who can’t take statins, ezetimibe alone still lowers LDL by 15-20% and reduces cardiovascular risk - just not as much as a statin would. But it’s the safest, cheapest, and most accessible option.
Why do some people feel worse on statins even after switching?
It could be the dose, the timing, or an underlying condition. Some patients need a lower dose, not a different drug. Others have undiagnosed hypothyroidism or vitamin D deficiency. A few have nocebo effects - they expect pain, so they feel it. That’s why clinics use blinded rechallenges and rule out other causes before concluding a patient is truly intolerant.
Can I take CoQ10 to reduce statin side effects?
Some patients report less muscle pain with CoQ10, but studies haven’t proven it consistently works. It’s not a substitute for proper protocol - but it’s low-risk and may help. Many clinics recommend 100-200 mg daily during rechallenge as a supportive measure, not a cure.
How long does it take to see results from a statin intolerance clinic?
Most patients get answers within 4-6 weeks. The initial break from statins takes 2 weeks. Testing and evaluation add another 1-2 weeks. Rechallenge and dose adjustments happen over the next 2-4 weeks. By week 6, most patients know if they can tolerate a statin again - and if not, what their next steps are.
Are statin intolerance clinics covered by insurance?
Yes - under Medicare Part B and most private plans. Lipid specialist visits are now covered for statin intolerance management since 2023. But coverage for non-statin drugs like PCSK9 inhibitors or bempedoic acid is trickier. Insurance often requires prior authorization and proof of statin failure. Clinics help with appeals - and many succeed.
What’s the success rate of statin intolerance clinics?
Cleveland Clinic’s 2022 data showed 68% of patients reached their LDL-C goal using their protocol. Hydrophilic statin switching worked for 72% of patients. Intermittent dosing helped 65%. Overall, 82% of patients in structured programs restarted lipid-lowering therapy, compared to just 45% in standard care.
Statin intolerance isn’t a dead end. It’s a puzzle - and clinics have the pieces. You don’t have to live with the fear of a heart attack just because your muscles hurt. There’s a better way.

Mimi Bos
December 28, 2025 AT 17:12i just tried rosuvastatin twice a week after my doc said i was statin intolerant and like??? it worked?? no muscle cramps and my ldl dropped like 30 points. i’m not even mad anymore lol
Payton Daily
December 30, 2025 AT 08:01let me tell you something real quick-this whole statin thing is a pharmaceutical scam. they don’t want you to know that vitamin d and magnesium fix everything. why do you think they push pills? because they make billions. i’ve been off statins for 7 years and my heart’s better than my 25-year-old nephew’s. the system is rigged. 🤡
Kelsey Youmans
December 31, 2025 AT 16:03While I appreciate the clinical rigor outlined in this piece, I must emphasize the importance of individualized patient care. The data presented-particularly the 82% success rate in structured programs-is compelling. However, access to lipid specialists remains inequitable, especially in rural and underserved communities. Systemic investment in training primary care providers in these protocols is not merely beneficial-it is ethically imperative.
Sydney Lee
January 1, 2026 AT 21:49Let’s be honest: most patients who claim statin intolerance are simply unwilling to endure mild discomfort for long-term survival. The idea that ‘muscle pain’ is a valid reason to forgo life-saving medication is a symptom of our culture’s pathological aversion to inconvenience. If you can’t tolerate a pill that prevents a heart attack, perhaps you shouldn’t be allowed to drive a car either. The data doesn’t lie-your laziness is killing you.
Debra Cagwin
January 1, 2026 AT 22:50If you’re reading this and you’ve been told you’re statin intolerant-please don’t give up. You’re not broken. You just haven’t found the right path yet. The fact that 72% of people can switch to a different statin? That’s hope. Twice-weekly dosing? That’s a win. Ask your doctor for a referral. Bring this article. You deserve to live without fear-and without pain. You’ve got this. 💪❤️
Hakim Bachiri
January 2, 2026 AT 10:54ok but why are we letting big pharma control our meds?? ezetimibe costs 35 bucks? but pcsk9 inhibitors are 6k?? that’s not science-that’s capitalism. also, why is no one talking about how the FDA is in bed with the drug companies? i’ve got a cousin who got denied coverage 4 times before they finally gave in. this isn’t medicine. it’s a pyramid scheme with lab coats.
Celia McTighe
January 3, 2026 AT 01:49OMG I just found out my mom got into a statin clinic and now she’s on rosuvastatin twice a week and she’s hiking again 😭 thank you for sharing this!! I’m crying happy tears. also-CoQ10 helped her too!! 🙌💖
Ryan Touhill
January 3, 2026 AT 19:32Interesting. But have you considered that the real issue isn’t statin intolerance-it’s the decline of American resilience? We’ve turned minor discomfort into a medical emergency. In my grandfather’s day, people took their medicine and didn’t complain. Now? We need clinics, gene tests, and appeals just to take a pill. We’ve become a nation of patients, not people. The solution isn’t more drugs-it’s more grit.
Teresa Marzo Lostalé
January 5, 2026 AT 04:20my grandma took statins for 12 years and never had side effects. then she switched to pravastatin after a bad reaction to simvastatin and lived to 98. point is: it’s not one-size-fits-all. but it’s also not a death sentence. take your time. ask questions. find your version of ‘working.’ 🌿