Smoking and Medications: How Cigarettes Alter Drug Levels Through Enzyme Induction
 Jan, 31 2026
Jan, 31 2026
When you smoke, your body doesn’t just absorb nicotine-it rewires how it processes medications. This isn’t a myth or a vague warning. It’s a well-documented, measurable, and sometimes dangerous change in your liver’s ability to break down drugs. For people taking medications like theophylline, clozapine, or even common pain relievers, smoking can slash drug levels by half. And when they quit? Those same drugs can suddenly build up to toxic levels-without any change in dosage.
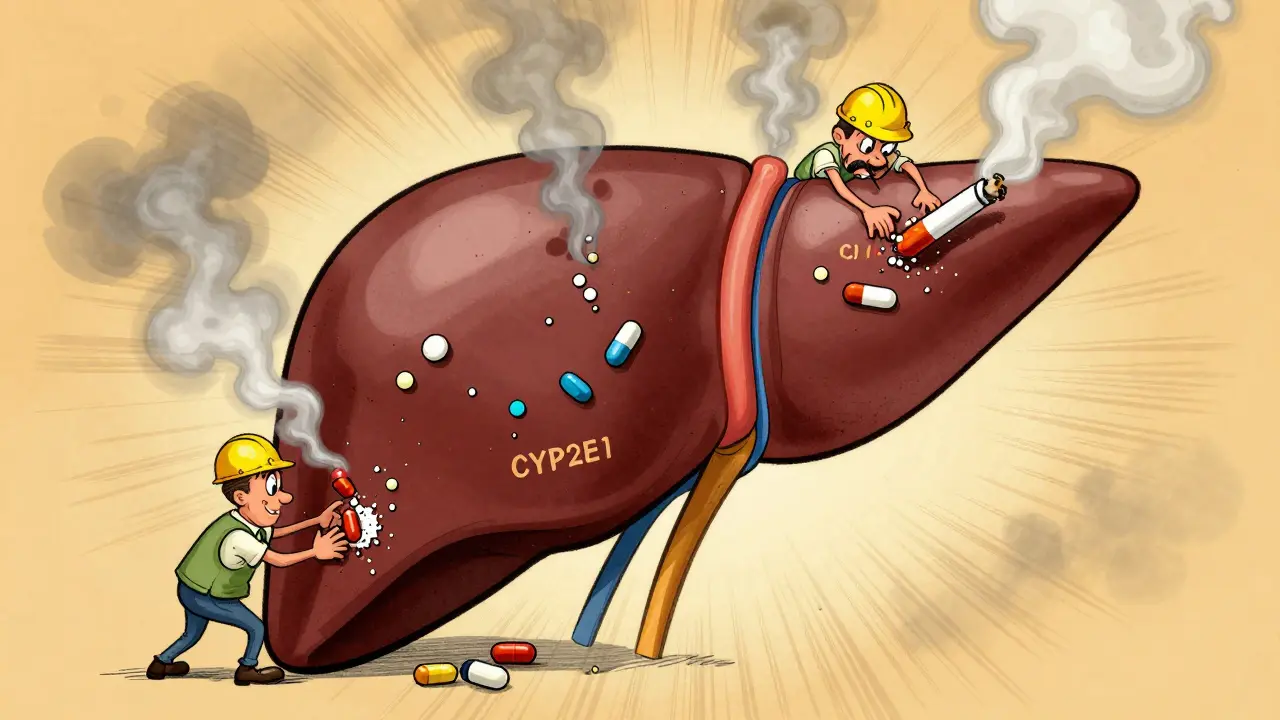
Why Smoking Changes How Drugs Work
Tobacco smoke contains chemicals called polycyclic aromatic hydrocarbons (PAHs). These aren’t just harmful to your lungs-they’re powerful signals to your liver. When PAHs enter your bloodstream, they bind to a receptor called AhR, which turns on genes that make more of certain liver enzymes. The biggest players here are CYP1A2, CYP1A1, CYP2E1, and some UGT enzymes. These enzymes are your body’s natural drug cleaners. More enzymes mean drugs get broken down faster-and leave your system before they can do their job.This isn’t subtle. Smokers clear caffeine 30-50% faster than non-smokers. That’s why some people who smoke need two or three cups of coffee just to feel awake. The same thing happens with prescription drugs. The effect builds slowly. After just a few days of smoking, enzyme levels start rising. Full induction takes about two weeks. But here’s the catch: it doesn’t matter if you smoke one cigarette or a pack a day. Once you hit 10 cigarettes daily, the enzyme boost plateaus. More smoke doesn’t mean more induction-it just means more damage to your lungs.
Drugs Most Affected by Smoking
Not all medications are affected equally. The ones at highest risk are those broken down primarily by CYP1A2. This enzyme handles about 15% of all commonly prescribed drugs. Here’s what you need to know:- Theophylline (used for asthma and COPD): Smokers clear it 58-100% faster. Their half-life drops from 8 hours to just 3 hours. Many smokers need nearly double the dose just to stay in the therapeutic range.
- Clozapine (an antipsychotic): A landmark 1994 study found smokers required 50% higher doses than non-smokers to achieve the same blood levels. Without this adjustment, the drug simply doesn’t work.
- Olanzapine (another antipsychotic): Clearance increases by 98% in smokers. Serum concentrations drop by 12%-enough to trigger relapse in schizophrenia patients.
- Duloxetine (an antidepressant): Smokers metabolize it 30% faster. This can lead to reduced effectiveness and worsening depression.
- Methadone: Even though it’s mainly processed by other enzymes, CYP1A2 handles a small but important part. Smokers clear it 15% faster, which can lead to withdrawal symptoms if doses aren’t adjusted.
- Acetaminophen (Tylenol): CYP2E1 breaks it down. Smokers process it faster, which might reduce pain relief-but also increases the risk of liver damage if they take too much.
Drugs like sertraline, fluoxetine, and propranolol are less affected because they rely on other enzymes (like CYP2D6). But don’t assume safety. Even small changes matter when you’re on a narrow therapeutic index drug-where the difference between effective and toxic is tiny.
The Hidden Danger: Quitting Smoking
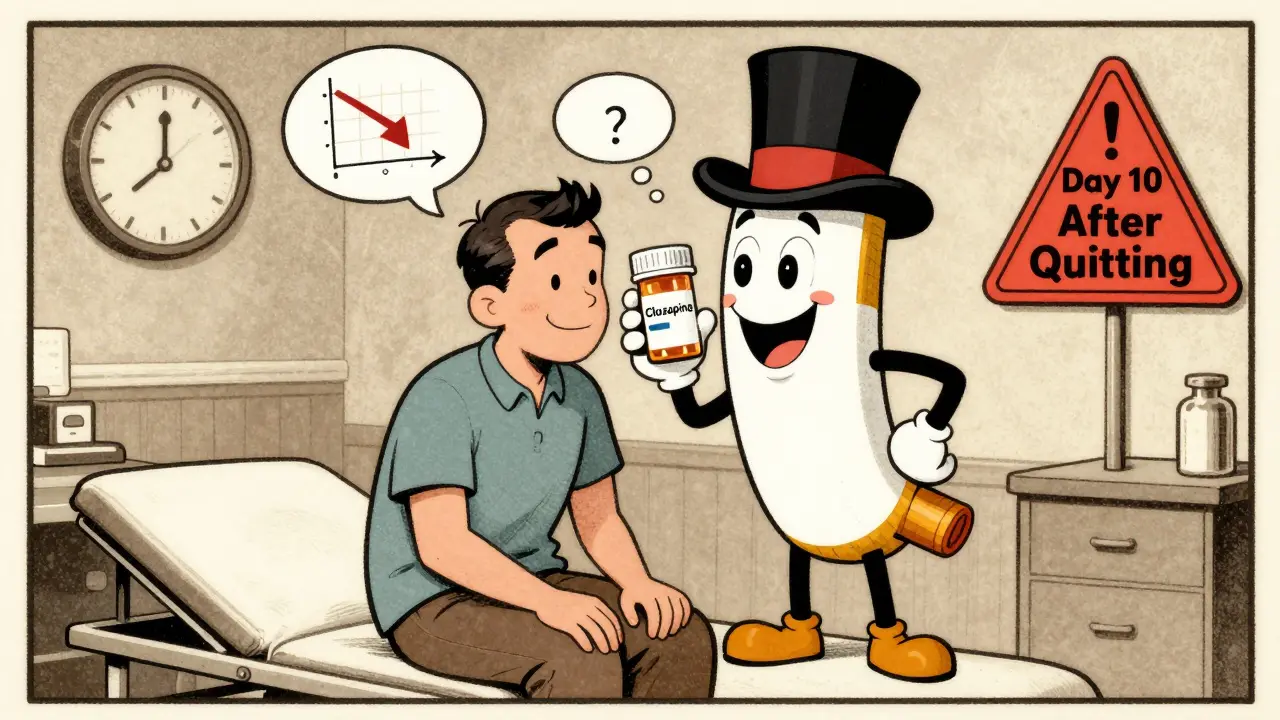
Most people think the risk ends when they stop smoking. It doesn’t. It gets worse.When you quit, your liver doesn’t instantly return to normal. Enzyme levels start dropping within 72 hours, but full reversal takes 2-4 weeks. During that time, your body is still clearing drugs at the same fast pace-but now, the drug dose you’ve been on for months is too high. The result? Toxic buildup.
There are real cases of people ending up in the hospital after quitting. One patient on theophylline had levels go from barely therapeutic to dangerously high-just 10 days after stopping smoking. No one changed the dose. No one warned them. The same thing happened with clozapine: the FDA’s database recorded 147 cases of toxicity after smoking cessation, with 89% occurring within two weeks.
Even common medications like pioglitazone (for diabetes) can cause problems. Smokers need higher doses. When they quit, their blood sugar can crash. One patient reported their A1C dropped from 7.8% to 5.9% after quitting-without changing diet or meds. That’s not a win. That’s hypoglycemia waiting to happen.
Why Doctors Often Miss This
A 2022 survey found only 37% of primary care doctors routinely check smoking status when prescribing theophylline. That’s alarming. This isn’t a rare edge case-it’s a routine clinical blind spot.Many providers assume smoking is just a lifestyle issue, not a pharmacological one. But the data doesn’t lie. The American Society of Health-System Pharmacists calls smoking a “major modifier” of drug metabolism. The FDA now requires drug labels to include tobacco interaction warnings for CYP1A2 substrates. And yet, it’s still not standard practice to ask patients about smoking when prescribing meds.
Pharmacists are seeing the fallout. On Reddit, a pharmacist shared a story of a patient hospitalized for theophylline toxicity after quitting smoking. Another wrote about adjusting clozapine doses for 12 patients in one month after they quit. These aren’t outliers. They’re predictable.

What You Should Do
If you smoke and take medication, here’s what you need to do:- Know your meds. Check if your drug is metabolized by CYP1A2. Common ones include clozapine, olanzapine, theophylline, duloxetine, and tizanidine. Ask your pharmacist or look up the drug’s prescribing information.
- Tell your doctor you smoke. Don’t assume they’ll ask. Say it upfront. “I smoke about X cigarettes a day.”
- If you’re quitting, talk to your doctor before you stop. Don’t wait until you feel sick. Ask: “Do I need to adjust my dose when I quit?”
- Get monitored. If you’re on a high-risk drug, ask for a blood level test before and after quitting. For theophylline or clozapine, this can be life-saving.
- Don’t assume your dose is “right.” If you’ve been on the same dose for years and recently quit smoking, your body is now handling that drug differently. Symptoms like dizziness, nausea, confusion, or low blood sugar could be signs of toxicity.
There’s a new tool called SmokeMetrix®-a simple breath test that measures how fast your body metabolizes caffeine to estimate CYP1A2 activity. It’s not widely available yet, but it’s a sign of where medicine is headed: personalized dosing based on real-time enzyme activity, not guesswork.
The Bigger Picture
This isn’t just about individual patients. It’s a systemic problem. In the U.S., over 34 million adults smoke. Among people with schizophrenia, nearly half do. In COPD and diabetes, smoking rates are far above average. That means thousands of people are on medications that don’t work-or are dangerously toxic-because no one asked about smoking.The cost? The AHRQ estimates $2.3 billion a year in preventable hospitalizations. Pharmaceutical companies like Pfizer spent $187 million in 2021 just managing the fallout from smoking-related dose changes in theophylline users.
The solution isn’t more drugs. It’s better communication. It’s asking the right question at the right time: “Do you smoke?” And then acting on the answer.
If you’re a smoker, your body is already under stress. Don’t let your meds add to it. If you’re thinking of quitting, don’t do it alone. Talk to your doctor or pharmacist. Your next dose might need to change-and it’s not your fault if it does.
Does smoking make all medications less effective?
No. Only medications broken down by specific liver enzymes-mainly CYP1A2, CYP2E1, and some UGTs-are affected. Common drugs like statins, most antibiotics, and many blood pressure medications are not significantly impacted. But for key drugs like clozapine, theophylline, and duloxetine, smoking can cut effectiveness in half.
How long after quitting smoking do drug levels change?
Enzyme activity starts dropping within 72 hours. The biggest shift happens between days 3 and 14 after quitting. That’s the critical window where drug levels rise fastest. Most toxicity cases occur during this time. Full normalization takes 2-4 weeks.
Can I just increase my dose if I smoke?
Never adjust your dose on your own. While smokers often need higher doses, increasing medication without medical supervision can lead to overdose if you quit later. Always work with your doctor or pharmacist. They’ll monitor your drug levels and adjust safely.
Are e-cigarettes or vaping the same as smoking?
Current evidence suggests vaping does not induce CYP1A2 or other drug-metabolizing enzymes the way tobacco smoke does. The key trigger-polycyclic aromatic hydrocarbons-is mostly absent in vape aerosols. So far, studies show no significant enzyme induction from vaping. But long-term data is still limited.
What should I do if I’m quitting smoking and on a high-risk medication?
Plan ahead. Talk to your prescriber at least a week before quitting. Ask if your medication needs a dose reduction. For drugs like clozapine or theophylline, a 25-50% reduction within 3-7 days of quitting is often needed. Monitor for side effects-drowsiness, dizziness, nausea, low blood sugar, or irregular heartbeat-and report them immediately.

Bryan Coleman
February 1, 2026 AT 08:38man i had no idea smoking could mess with my meds like this. i’ve been on duloxetine for years and just quit last month-suddenly i was dizzy as hell and felt like i was drunk without drinking. my doc didn’t say a word. guess i’m lucky i didn’t end up in the er.
Naresh L
February 1, 2026 AT 09:08it’s fascinating how a simple habit like smoking can alter biochemistry at the molecular level. the body is not just a machine-it’s a dynamic ecosystem where even external toxins become signals. what’s more troubling is how medicine still treats smoking as a moral failing rather than a pharmacokinetic variable. we diagnose, we prescribe, but we rarely ask: ‘what are you exposing yourself to?’
Sami Sahil
February 2, 2026 AT 04:56bro this is wild 😳 i smoke 10 a day and take zoloft-never thought it’d affect me. just got my dose bumped up last week cause i ‘wasn’t responding’… turns out i was just burning it up too fast. gonna tell my doc next visit. ty for the heads up!!