Presumed Consent in Pharmacy: When Pharmacists Can Swap Brand Drugs for Generics Without Asking
 Dec, 19 2025
Dec, 19 2025
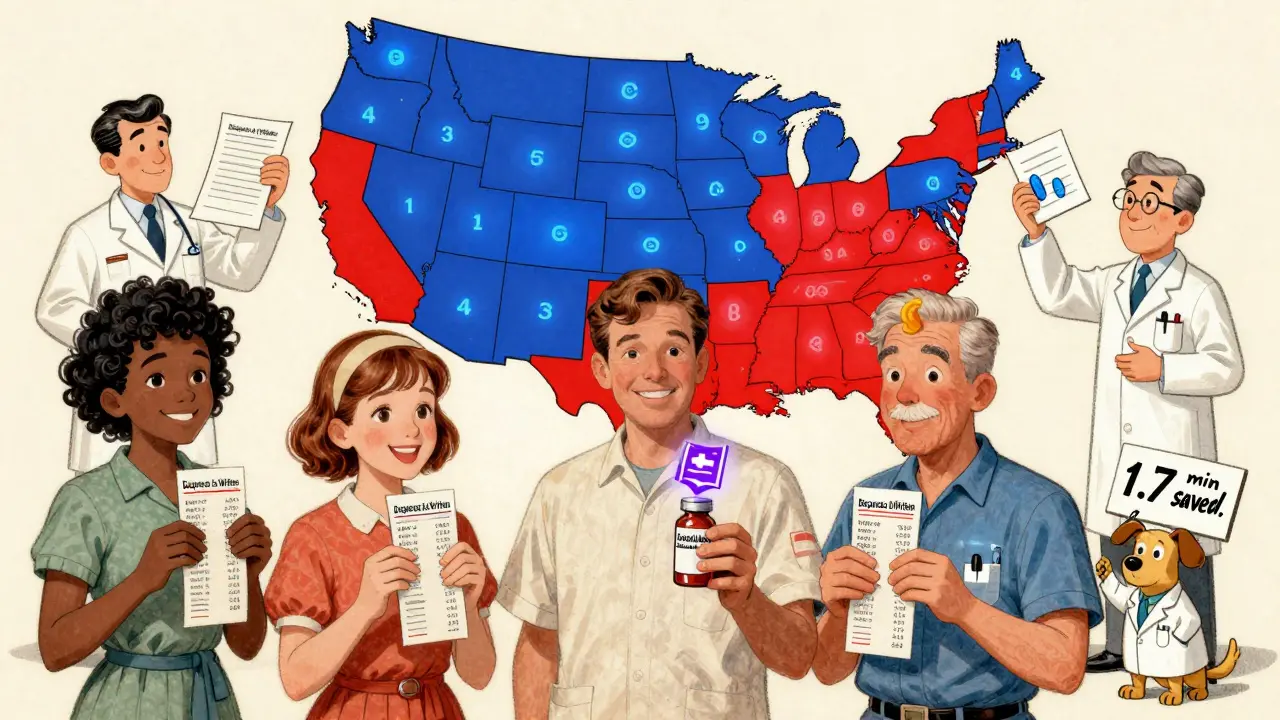
Every time you pick up a prescription, there’s a good chance the pharmacist handed you a generic version instead of the brand-name drug your doctor wrote on the script. You might not have noticed. You probably didn’t sign anything. That’s because in 43 states, pharmacists are allowed to make that switch without asking you first. This is called presumed consent.
What Presumed Consent Actually Means
Presumed consent doesn’t mean pharmacists can swap any drug for any other. It means that if a generic version of your medication is available, approved by the FDA as therapeutically equivalent, and not blocked by your doctor or state law, the pharmacist can dispense it without getting your verbal or written approval at the counter. The law assumes you’re okay with it - because generics save money, work the same way, and are just as safe for most people. The FDA’s Orange Book is the official list that tells pharmacists which generics are approved as interchangeable with brand drugs. These are marked with an "A" rating. If your drug has an "A" rating, it’s cleared for substitution. That’s the foundation of the whole system.How It Works in Practice
Let’s say your doctor prescribes Lipitor for cholesterol. The pharmacist sees that a generic version called atorvastatin is available, cheaper, and rated "A" by the FDA. In a presumed consent state, they can fill your prescription with the generic without saying a word. They don’t need to ask, “Do you mind if I give you the generic?” But here’s the catch: most states still require them to tell you afterward. That notice might come on the label, in a printed sheet, or through an automated phone call. It’s not always obvious, and many people never realize the switch happened - until they see the price difference on their receipt. In 19 states, pharmacists are actually required to substitute generics when possible. That’s called mandatory substitution. In the other 31, they can choose to substitute, but aren’t forced to. Presumed consent is about permission, not obligation. Even in mandatory states, if your doctor writes "dispense as written" or "no substitution," the pharmacist must follow that.Why This System Exists
The goal is simple: save money. Generic drugs cost, on average, 80-85% less than their brand-name counterparts. In 2022, generics made up 90% of all prescriptions filled in the U.S. - but only 15% of total drug spending. That’s a $1.68 trillion savings over the past decade, according to the Association for Accessible Medicines. Without presumed consent, every substitution would require a phone call, a signature, or a delay. That slows down pharmacies, increases costs, and creates friction in the system. A 2022 study by the American Society of Health-System Pharmacists found that presumed consent cuts prescription processing time by about 1.7 minutes per script. Multiply that across millions of prescriptions, and you’re talking nearly $3 billion saved in labor costs each year. It’s not just about pharmacies. It’s about patients too. Medicare Part D beneficiaries save an average of $627 per year thanks to generic substitution. For people on fixed incomes, that’s rent, groceries, or insulin.Where It Gets Complicated
Not all drugs are created equal. Some medications have what’s called a narrow therapeutic index - meaning the difference between an effective dose and a harmful one is very small. Small changes in how the drug is absorbed can lead to serious problems. Drugs like warfarin (a blood thinner), levothyroxine (for thyroid), and certain anti-seizure medications fall into this category. The American Epilepsy Society documented 178 cases of breakthrough seizures between 2018 and 2022 linked to generic substitutions. As a result, 15 states - including Tennessee and Hawaii - have special rules. In those states, pharmacists can’t substitute these drugs without explicit patient consent, even in presumed consent states. Biosimilars - the newer, more complex versions of biologic drugs like Humira or Enbrel - add another layer. Only 46 states allow automatic substitution of interchangeable biosimilars. Four states - North Carolina, Oklahoma, Pennsylvania, and Texas - ban it entirely. Why? Because these drugs are made from living cells, not chemicals. Their manufacturing is harder to replicate exactly, and the FDA’s standards for interchangeability are stricter.What Pharmacists Have to Juggle
Pharmacists aren’t just dispensing pills. They’re navigating 51 different sets of rules - one for each state plus Washington, D.C. That’s a nightmare for anyone working across state lines or running a chain pharmacy. They need to know:- Which drugs are substitutable (based on the FDA’s Orange Book)
- Which drugs are off-limits in their state (like antiepileptics or blood thinners)
- Whether they need to notify the patient after substitution
- What documentation is required (electronic logs, printed notices, etc.)
- Whether the prescriber blocked substitution
What Patients Really Think
Most patients don’t mind - if they even notice. On Drugs.com, 68% of 1,243 comments about generic substitution were positive. People wrote things like, “Saved me $45 a month,” or “I didn’t feel any difference.” But the 22% who complained? Their stories are real. One man in Tennessee said his seizure medication stopped working after a switch. Another said his blood pressure spiked after switching generics. These aren’t rare cases. They’re the reason some states added restrictions. Reddit threads from pharmacists tell the same story. One user in Ohio wrote: “95% of patients don’t care. The other 5%? They lose trust in the whole system.” That’s the trade-off. Efficiency for most, anxiety for some.The Future of Presumed Consent
The system isn’t staying the same. States are updating their laws - fast. New York now requires all substitutions to be documented electronically. California expanded notification rules for biosimilars in 2022. The FDA is working on clearer guidelines for biologic substitution. And 17 states are considering a new model law called the “Uniform State Substitution Act,” which would standardize rules across state lines. The big question: Should presumed consent apply to all drugs? Experts are split. Dr. Erika Lietzan, a leading pharmaceutical law scholar, says it’s the most efficient system we have - but only if notification is clear and consistent. Dr. Jerry Avorn from Harvard argues that for certain high-risk drugs, presumed consent is dangerous. The emerging consensus? A tiered system. Presumed consent for most drugs - but explicit consent for those with narrow therapeutic indices. That’s already happening in 15 states. More will follow.What You Can Do
You don’t have to be passive about this. Here’s how to take control:- Check your prescription label. If the name doesn’t match what your doctor wrote, ask if it was substituted.
- Look for a notice - it might be on the bag, the receipt, or in your pharmacy’s app.
- If you’re on a drug with a narrow therapeutic index (like warfarin, levothyroxine, or anti-seizure meds), ask your pharmacist: “Is substitution allowed here?”
- Ask your doctor to write “dispense as written” on your prescription if you want the brand.
- Keep a list of your medications and which versions you’ve taken. If you feel different after a switch, report it.
Can my pharmacist switch my medication without telling me?
In 43 states, pharmacists can substitute generic drugs without asking you first - but they are required to notify you after the fact. That notice might be on the label, a printed sheet, or through your pharmacy’s app. You may not notice it unless you’re looking for it.
Are generic drugs really the same as brand-name drugs?
For most drugs, yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also meet the same quality and safety standards. The only differences are in inactive ingredients like fillers or dyes, which rarely affect how the drug works.
Which drugs can’t be substituted without my permission?
Drugs with a narrow therapeutic index - where small changes in blood levels can cause harm - often have restrictions. These include warfarin, levothyroxine, and anti-seizure medications like phenytoin or carbamazepine. Fifteen states require explicit consent before substituting these drugs, even in presumed consent states.
Why do some states require consent and others don’t?
It’s a mix of history, politics, and patient safety concerns. States with presumed consent prioritize efficiency and cost savings. States requiring explicit consent prioritize patient autonomy and worry about rare but serious side effects. There’s no national standard - so rules vary depending on where you live.
Can I ask for the brand-name drug even if a generic is available?
Yes. You can always ask your pharmacist for the brand-name version. They may need to check with your insurance, and you might pay more out of pocket. If you want to make sure you always get the brand, ask your doctor to write “dispense as written” or “no substitution” on the prescription.
Do biosimilars follow the same rules as generics?
No. Biosimilars are more complex and are treated differently. Only 46 states allow automatic substitution of interchangeable biosimilars. Four states - North Carolina, Oklahoma, Pennsylvania, and Texas - ban it entirely. Pharmacists must check the FDA’s Purple Book for biosimilar rules, not the Orange Book.

Nancy Kou
December 21, 2025 AT 06:09Pharmacists swapping generics without asking is just common sense. I’ve been on the same meds for 12 years, switched to generic, saved $800 a year, and never felt a thing. Why should I pay extra for marketing and fancy packaging that does the exact same thing?
Alana Koerts
December 22, 2025 AT 04:08Let’s be real - this system works until someone’s seizure meds stop working because some pharmacist decided to save a buck. The FDA says they’re equivalent but they’re not. The fillers change absorption rates. People die from this. And no one takes responsibility.
Hussien SLeiman
December 22, 2025 AT 08:15Look, I get the cost savings. I really do. But this whole presumed consent thing is just corporate convenience dressed up as patient care. You don’t get to assume consent for something that affects your brain chemistry. It’s not like swapping coffee brands. One person’s ‘same thing’ is another person’s nightmare. And don’t give me that ‘95% don’t care’ crap - the 5% who do care are the ones getting screwed over. And yeah, I’ve seen it. My cousin went from stable to crashing after a switch. No warning. No consent. Just a cheaper pill and a trip to the ER. This isn’t efficiency. It’s negligence with a spreadsheet.
Edington Renwick
December 23, 2025 AT 22:07They’re not even required to tell you properly. I got my refill, saw the label change, called the pharmacy, and they said ‘oh yeah, we switched it last month.’ No email. No text. No nothing. And now my insurance won’t cover the brand even though I asked for it. This isn’t a system - it’s a trap.
Kathryn Featherstone
December 23, 2025 AT 23:13If you’re on warfarin, levothyroxine, or anything with a narrow therapeutic index, never assume. Always ask. Always check the label. Always keep a list. Your pharmacist isn’t your enemy - they’re just caught in a broken system. But you’re the only one who can protect yourself. Write ‘dispense as written’ on your script. It takes 5 seconds. It could save your life.
Sarah McQuillan
December 25, 2025 AT 07:42Canada does this too and no one’s freaking out. We’ve had generics for decades. People here don’t care because they trust the system. If you’re from the US and you’re scared, maybe it’s not the law - it’s the lack of transparency. Fix the notification system, not the substitution rule.
Aadil Munshi
December 26, 2025 AT 18:03Interesting how the same people who scream about bodily autonomy when it comes to vaccines are totally fine with pharmacists swapping your brain-altering meds without a word. Consistency is a myth, isn’t it? The real issue isn’t substitution - it’s that we’ve outsourced our health decisions to bureaucrats and corporate cost-cutters and now we’re surprised when the system fails. Welcome to neoliberal healthcare. You’re doing great.
Chris porto
December 28, 2025 AT 08:54It’s not about whether generics are safe. It’s about whether we trust people to make decisions about their own bodies. If the law assumes consent, then we’re saying your body doesn’t belong to you - it belongs to the system. And that’s a dangerous precedent. Even if 99% of people are fine, the 1% who aren’t? They’re the ones who get erased by the algorithm.
Alisa Silvia Bila
December 28, 2025 AT 18:13Check your label. Always. It’s that simple.