Oral Food Challenges: Safety and Diagnostic Value
 Dec, 24 2025
Dec, 24 2025
When a child breaks out in hives after eating peanut butter, or an adult gets stomach cramps after drinking milk, it’s natural to assume they have a food allergy. But here’s the problem: most of the time, they don’t. Skin prick tests and blood tests for IgE antibodies can be wrong up to half the time. That’s why doctors rely on something far more accurate - the oral food challenge.
Why the Oral Food Challenge Is the Gold Standard
No other test can say for sure whether you’re truly allergic to a food. Skin tests show if your body has antibodies, but those antibodies don’t always mean you’ll react when you eat the food. Blood tests measure antibody levels, but even high numbers don’t guarantee a reaction. That’s why the American Academy of Allergy, Asthma & Immunology (AAAAI) and the European Academy of Allergy and Clinical Immunology (EAACI) both call the oral food challenge the gold standard. An oral food challenge isn’t just another test. It’s a real-life test. You eat the food - slowly, under medical supervision - and doctors watch to see what happens. If you react, they treat it right away. If you don’t, you get a clear answer: you’re not allergic. This is the only way to know for sure. In the U.S., about 32 million people have food allergies. But studies show that up to 80% of people who think they’re allergic to foods like milk, eggs, or wheat actually aren’t. Without an oral food challenge, they stay on restrictive diets for years - missing out on nutrition, social events, and peace of mind.How an Oral Food Challenge Works
The process is simple in theory, but tightly controlled in practice. You start with a tiny amount - as little as 1 to 2 milligrams of the food. That’s about the size of a grain of sand. If there’s no reaction after 15 to 30 minutes, you get a slightly bigger dose. This continues until you’ve eaten a full serving, or until a reaction occurs. The whole thing takes 3 to 6 hours. You’re monitored the entire time. Your heart rate, breathing, skin, and digestion are checked regularly. The food can be given in many forms: as peanut butter, baked into a muffin, or even in a capsule so you can’t taste it. The goal is to mimic real-life exposure as closely as possible. Most challenges are done in an “open” format - meaning both you and the doctor know what food you’re eating. This is the most common because it’s practical. In rare cases, like when anxiety might affect the result, a double-blind challenge is used. That means neither you nor the doctor knows if it’s the real food or a placebo. These are mostly done in research settings.What Happens If You React?
It’s natural to be nervous. You’re eating something you’ve been told could kill you. But here’s the truth: severe reactions are rare. About 40% to 60% of oral food challenges result in mild symptoms - things like a few hives, a flushed face, or a slightly itchy mouth. These are easy to treat with antihistamines and usually resolve within minutes. Only 1% to 2% of challenges lead to a reaction that requires epinephrine. That’s lower than the risk of many common medical procedures. And because everything happens in a clinic with emergency equipment and trained staff on-site, even those rare reactions are handled safely. Dr. Laura Capucilli, an allergist in Rochester, says, “Severe reactions during oral food challenges are uncommon. If a reaction occurs, most are mild and involve hives or flushing. They can be reacted right in the office setting.” The key is preparation. You can’t take antihistamines for 5 to 7 days before the test - they can hide early signs of a reaction. You also shouldn’t be sick. If you have a cold or asthma flare-up, the challenge gets postponed. Respiratory infections can make reactions worse.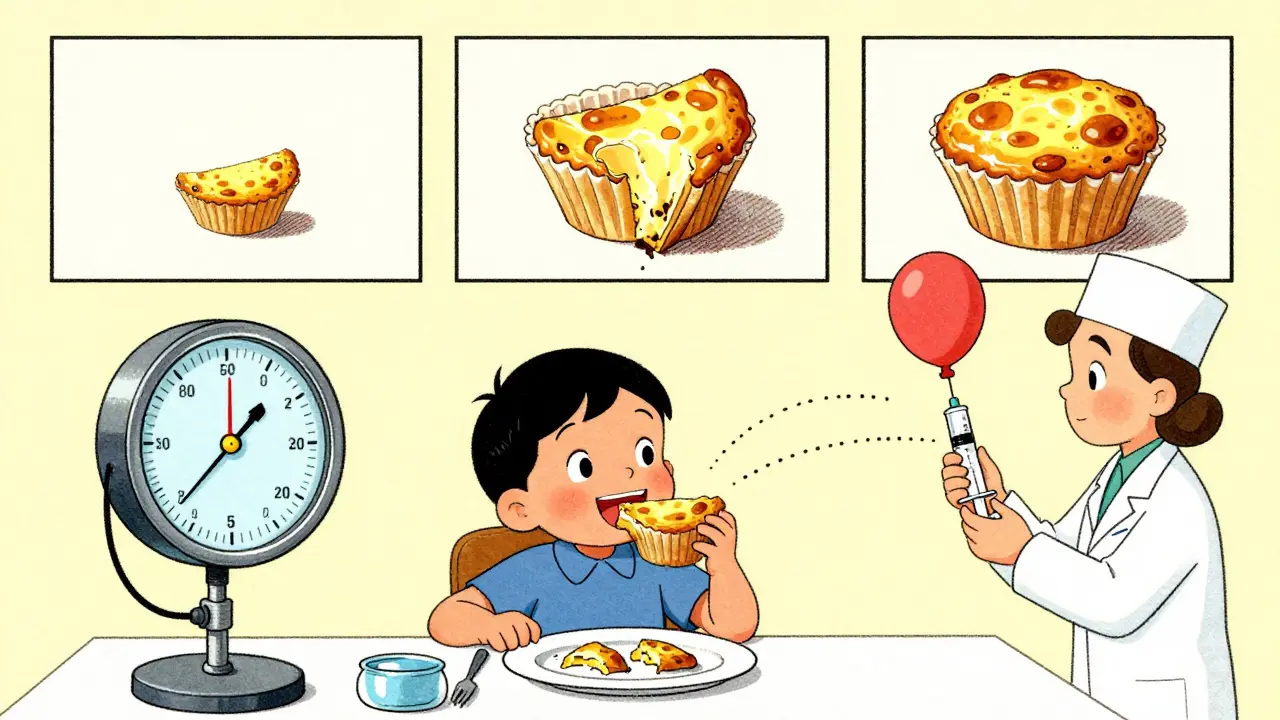
Who Benefits the Most?
Oral food challenges aren’t for everyone. They’re not a screening tool. If you’ve had a severe reaction like anaphylaxis in the past, you don’t get tested this way. It’s too risky. But they’re perfect for three situations:- You’ve had a positive test, but you’ve never had a real reaction - or your reaction was mild.
- You think you’ve outgrown an allergy - especially common with milk, egg, soy, and wheat allergies in children.
- Your doctor suspects your allergy diagnosis might be wrong.
What About Other Tests?
There are newer tests like component-resolved diagnostics. These look at specific proteins in foods instead of the whole food. They’re more precise than traditional blood tests - but still not perfect. Studies show they’re about 85% accurate at predicting reactions. That sounds good - until you realize the oral food challenge is nearly 100% accurate. No other test comes close. Even the best blood test can’t tell you how much of a food you can safely eat. Only an oral food challenge can show your personal threshold. That’s important for people who can tolerate small amounts but react to larger ones. And while companies like Thermo Fisher Scientific market these advanced blood tests, they’re still used as supporting tools - never replacements.The Psychological Side
The fear around food allergies is real. Parents worry constantly. Kids grow up avoiding birthday cakes, school lunches, and family dinners. That stress doesn’t disappear just because a test says you’re allergic. Surveys show 78% of parents feel moderate to high anxiety before an oral food challenge. Kids cry. Some refuse to eat. But after the test? The numbers flip. Nearly 90% of families say they’re satisfied with the outcome - even if the result was positive. Why? Because uncertainty is worse than a confirmed diagnosis. Knowing you’re allergic means you can prepare. Knowing you’re not allergic means you can live freely. Practical tips from families who’ve been through it: bring your child’s favorite toy or tablet. Wear loose clothes. Don’t schedule the test on a school day. Make sure your child sleeps well the night before. And don’t skip the pre-challenge counseling - it helps more than you think.

Winni Victor
December 25, 2025 AT 21:44Okay but have you ever tried to get an oral food challenge covered by insurance? Good luck. My kid’s allergist said it’s ‘not medically necessary’ even though we’ve been avoiding eggs for 4 years and she’s never had more than a rash. Now we’re paying $800 out of pocket to find out if she can eat scrambled eggs. I’m not mad, I’m just disappointed.
sagar patel
December 26, 2025 AT 03:51Oral food challenge is gold standard because it tests real world exposure not theoretical antibody presence
Ben Harris
December 27, 2025 AT 06:45So you’re telling me we’re risking kids eating peanut butter in a clinic because some doctor’s ego needs to feel like they’re doing science instead of just prescribing epinephrine pens and calling it a day? I’ve seen parents cry over this test and the allergist just smiles like they’re hosting a cooking show
Also why is it always peanut butter? Why not test with a full sandwich? Or a cookie? Or a burrito? Real life isn’t a lab test it’s chaos
And don’t get me started on the ‘you can’t take antihistamines’ rule. My daughter got a cold the week before and we had to reschedule. So now we’re stuck in limbo for another 6 months while she misses her cousin’s birthday party because ‘we don’t know if she’s allergic to cake’
It’s not a challenge it’s a performance
Zabihullah Saleh
December 28, 2025 AT 20:30There’s something deeply human about this whole process. We’ve outsourced our relationship with food to labs and algorithms - IgE levels, component diagnostics, predictive models - but in the end, the body still has to speak for itself. The oral food challenge is a quiet act of trust: trust in the body’s ability to tell the truth, trust in the doctor’s restraint, trust that a grain of sand can change a life.
It’s not just medicine. It’s ritual.
Think about it: you’re sitting there, watching your child eat something you’ve been told could kill them, and you’re holding your breath not because you fear death - but because you fear the silence after. The silence where the fear ends and freedom begins.
I’ve met parents who cried after a negative result. Not from relief. From grief. Grief for the years they lost. Grief for the birthday cakes they didn’t bake. Grief for the playgrounds they avoided.
Maybe the real miracle isn’t the test. It’s the fact that we still let people eat.
Lindsay Hensel
December 30, 2025 AT 16:13Thank you for this comprehensive and deeply compassionate overview. The psychological burden of food allergies is profoundly underdiscussed, and your emphasis on the emotional toll - both pre- and post-challenge - is both accurate and necessary.
It is imperative that clinicians prioritize pre-test counseling, not as an afterthought, but as a core component of care. The reduction in parental anxiety post-challenge, even with a positive result, speaks volumes about the value of certainty over ambiguity.
I urge all healthcare providers to advocate for insurance coverage and accessibility improvements. This is not a luxury. It is a medical necessity.
Sophie Stallkind
December 31, 2025 AT 07:19While the oral food challenge remains the diagnostic gold standard, its implementation remains inconsistent across geographic and socioeconomic lines. In rural communities, access to board-certified allergists with proper emergency protocols is severely limited.
Furthermore, the current guidelines permitting home-based challenges for low-risk cases, while innovative, require rigorous oversight. Without standardized protocols and mandatory remote monitoring, such practices may introduce unintended risks.
Policy reform must accompany clinical advancement. We cannot allow diagnostic accuracy to be a privilege of urban centers and private insurance.
Katherine Blumhardt
January 1, 2026 AT 22:58my kid did the peanut challenge and she cried the whole time and i cried too and then she ate the whole peanut butter cup and didnt die and now shes eating pb&j every day and i just wanna say thank you to the doctors who did this because i was so scared
also the nurse gave her a sticker and that helped
Michael Dillon
January 3, 2026 AT 19:33Let’s be real - the whole oral food challenge thing is just a fancy way of saying ‘we don’t trust your test results so let’s make you eat your worst fear’
Meanwhile, the same doctors who say ‘only OFC is accurate’ are the ones selling you $500 blood tests every year. Coincidence? I think not
And why is it always peanuts and eggs? What about soy? Wheat? Shellfish? You know what’s way more common than peanut allergies? Being broke and having to eat cheap processed food. But nobody’s running a challenge for that
Also why is the ‘no antihistamines’ rule so strict? My cousin took Benadryl before and still got a rash - so what? Maybe the test is too sensitive
It’s not science. It’s theater with a clipboard
Gary Hartung
January 4, 2026 AT 05:15Let me just say - the fact that we’re still relying on a 1950s-era method - feeding people food and watching them - while we have AI-powered immune profiling, CRISPR-based diagnostics, and machine learning models trained on millions of patient records - is nothing short of a national disgrace.
Dr. Nadeau says ‘OFC will remain the gold standard for the foreseeable future’ - and I say: ‘foreseeable’ is not ‘acceptable.’
We are in the 21st century. We have satellites orbiting Mars. We have neural implants helping paralyzed people walk. And yet, to diagnose a peanut allergy, we make a child eat a spoonful of paste while five nurses hover like a SWAT team?
It’s not ‘gold standard.’ It’s a relic. A beautiful, necessary relic - but a relic nonetheless.
And until we invest in real innovation - not just ‘home-based’ tweaks - we’re not healing families. We’re just babysitting fear.