Hydrochlorothiazide vs Alternatives: Pros, Cons, and Best Choices
 Oct, 23 2025
Oct, 23 2025
Diuretic Selection Tool
Your Health Profile
Select all conditions that apply to you
Recommendations
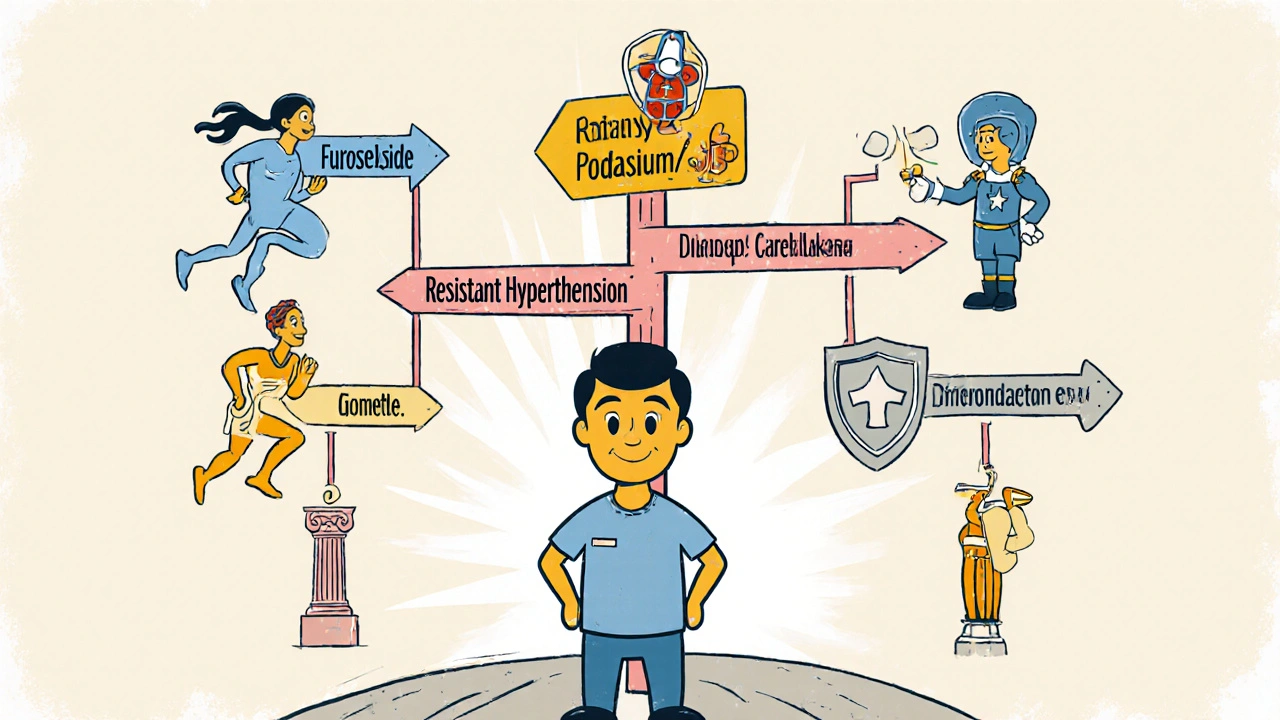
When your doctor mentions a water‑pill for high blood pressure or swelling, the name Hydrochlorothiazide often pops up. But you might wonder if there’s a better fit for your health profile. This guide breaks down how that drug works, weighs its strengths against the most common substitutes, and helps you pick the right option for conditions like hypertension, edema, or gout.
How Hydrochlorothiazide Works
Hydrochlorothiazide is a thiazide‑type diuretic that blocks the sodium‑chloride transporter in the distal convoluted tubule of the kidney. By preventing sodium reabsorption, it draws water into the urine, reducing blood volume and lowering blood pressure. The effect also lowers calcium excretion, which is why doctors sometimes favor it for patients at risk of kidney stones.
Key Benefits and Drawbacks of Hydrochlorothiazide
Benefits include a low cost, once‑daily dosing, and a proven track record in large‑scale hypertension trials. It can be combined safely with many other blood‑pressure drugs, making it a staple in combination pills.
Drawbacks center on metabolic side effects: potassium loss, elevated uric acid (triggering gout attacks), and a modest rise in blood glucose. Some people experience increased sensitivity to sunlight or a mild rise in cholesterol. Because it works mainly in the distal tubule, it’s less potent for rapid fluid removal than loop diuretics.
Top Alternatives - Quick Overview
Chlorthalidone is a thiazide‑like diuretic that acts farther downstream in the nephron, offering a longer half‑life and stronger blood‑pressure reduction.
Indapamide blends thiazide action with vasodilatory properties, making it gentler on electrolyte balance while still effective for hypertension.
Furosemide is a loop diuretic that works in the thick ascending limb, delivering rapid, high‑volume fluid removal for edema or acute heart failure.
Spironolactone blocks aldosterone receptors, providing potassium‑sparing diuresis and added benefit in resistant hypertension.
Losartan is an angiotensin‑II receptor blocker (ARB) that isn’t a diuretic but is often paired with thiazides to improve blood‑pressure control without adding potassium loss.
Side‑Effect Comparison Table
| Medication | Potassium Impact | Uric Acid | Blood‑Sugar Rise | Typical Use Cases |
|---|---|---|---|---|
| Hydrochlorothiazide | ↓ (risk of hypokalemia) | ↑ (gout risk) | ↑ modestly | Hypertension, mild edema |
| Chlorthalidone | ↓ (slightly more than HCTZ) | ↑ similar | ↑ modestly | Hypertension, resistant cases |
| Indapamide | Neutral to slight ↑ (potassium‑sparing) | Neutral | Neutral | Hypertension, metabolic syndrome |
| Furosemide | ↓ (strong) | Variable | May increase | Acute edema, heart failure |
| Spironolactone | ↑ (potassium‑sparing) | Neutral | Neutral | Resistant hypertension, primary aldosteronism |
| Losartan | Neutral | Neutral | Neutral | Hypertension, diabetic nephropathy |
Choosing the Right Diuretic for Your Situation
Start by asking what you need the pill to do. If the goal is long‑term blood‑pressure control with minimal daily dosing, Hydrochlorothiazide or Chlorthalidone are the go‑to choices. For patients who also have gout or borderline low potassium, Indapamide often feels gentler because it doesn’t drop potassium as sharply. When rapid fluid removal is critical-such as in decompensated heart failure-Furosemide outperforms thiazides by a wide margin. If you’ve already hit a blood‑pressure ceiling on a thiazide and need extra control without more potassium loss, adding Spironolactone can lower readings by 5‑10 mmHg and also protect the kidneys. For patients with diabetes or chronic kidney disease, an ARB like Losartan paired with a low‑dose thiazide gives solid pressure drops while sparing the kidneys from additional stress. In practice, the decision tree looks like this:
- Is fast‑acting fluid removal needed? → Choose Furosemide.
- Do you have a history of low potassium or gout? → Prefer Indapamide or add a potassium‑sparing agent.
- Is resistant hypertension the problem? → Step up to Chlorthalidone or combine with Spironolactone.
- Do you need kidney protection for diabetes? → Add Losartan to a low‑dose thiazide.
Practical Tips for Switching or Adding a Diuretic
- Check baseline electrolytes (especially potassium and magnesium) before any change.
- Schedule follow‑up labs 1-2 weeks after starting a new diuretic to catch early shifts.
- If moving from Hydrochlorothiazide to Chlorthalidone, use a 1:1 dose conversion (25 mg HCTZ ≈ 12.5 mg chlorthalidone) and monitor blood pressure weekly.
- Combine a thiazide with a potassium‑rich diet (bananas, oranges, leafy greens) or a low‑dose supplement if labs dip.
- Never stop a loop diuretic abruptly in heart‑failure patients; taper over several days to avoid rebound fluid retention.
Frequently Asked Questions
Can I take Hydrochlorothiazide and a potassium supplement together?
Yes, many clinicians add a low‑dose potassium chloride (typically 8-20 mEq) when the diuretic drives potassium below 3.5 mmol/L. Always check blood work first.
Why would a doctor switch me from Hydrochlorothiazide to Indapamide?
Indapamide tends to cause fewer electrolyte swings and may be better for patients with gout, diabetes, or borderline low potassium.
Is Hydrochlorothiazide safe during pregnancy?
It’s classified as Category B, meaning animal studies show no risk but human data are limited. Most obstetricians prefer other agents unless blood‑pressure control is essential.
What’s the main difference between a thiazide and a thiazide‑like diuretic?
Thiazides (e.g., Hydrochlorothiazide) act directly on the sodium‑chloride transporter, while thiazide‑like drugs (e.g., Chlorthalidone, Indapamide) bind elsewhere, giving a longer duration and sometimes stronger pressure‑lowering effects.
Can I replace Hydrochlorothiazide with a non‑diuretic blood‑pressure pill?
Often, doctors add an ACE inhibitor, ARB, or calcium‑channel blocker instead of a diuretic, especially if kidney function is a concern. The choice depends on overall cardiovascular risk.

Suraj 1120
October 23, 2025 AT 21:11Hydrochlorothiazide is cheap, but it’s often a lousy fit for patients with gout.
Shirley Slaughter
November 4, 2025 AT 09:58Reading through the breakdown, it’s clear that the “one‑size‑fits‑all” myth falls apart fast. The author does a solid job highlighting that chlorthalidone hangs on longer and can knock the pressure down more reliably. If you’re juggling gout, indapamide’s gentler potassium profile is a lifesaver. And let’s not forget how a simple potassium‑rich diet can offset a lot of the HCTZ pitfalls.
Sean Thomas
November 15, 2025 AT 23:45Honestly, the pharma lobby wants us to believe every pill is a miracle, but the data says otherwise. The table shows HCTZ’s potassium drain, which is a perfect setup for the “hidden agenda” of chronic disease manufacturers. If you’re wary of big‑drug narratives, consider that chlorthalidone’s longer half‑life was discovered by a small‑scale university lab, not a marketing committee. And the fact that indapamide sneaks in vasodilation suggests they’re trying to mask cardiovascular risk with a fancy label.
Aimee White
November 27, 2025 AT 13:31Step into the rabbit hole, folks: the calcium‑saving side‑effects of indapamide are a whisper of the “real” story hidden in the fine print. The author’s chart is a clue-look at the neutral uric acid line, that’s no accident. While the mainstream touts HCTZ for stone prevention, the subtle shift in sodium‑chloride transport is a gateway for the body’s own mineral balancing tricks, a cascade the pharma folks don’t want us to see. In short, read the fine print, the devil’s in the diuretic details.
Javier Muniz
December 9, 2025 AT 03:18Great summary! If you’re thinking about switching, start with a low‑dose trial of indapamide and keep an eye on your labs. A banana a day or a splash of orange juice can help keep potassium steady. And remember, you don’t have to jump straight to a loop diuretic unless you’re in acute heart‑failure.
Sarah Fleming
December 20, 2025 AT 17:05The author’s “switch” suggestion sounds innocent, but who decides when a switch is needed? The hidden hand behind the scenes pushes chlorthalidone because it’s older, cheaper, and easier to market worldwide. The table’s “Potassium Impact” column is a thin veil-don’t be fooled by the mild “↓” sign; it’s a gateway to chronic electrolyte chaos.
Debra Johnson
January 1, 2026 AT 06:51It is imperative that patients understand the moral weight of medication choices; choosing a cheap diuretic simply because it is inexpensive can betray one's health responsibilities. The table presented is accurate, yet it omits the ethical dimension of long‑term renal impact. One must critically evaluate whether a short‑term cost‑saving is justified when it may precipitate future kidney injury. Therefore, proactive monitoring and informed consent are not optional-they are essential.
Andrew Wilson
January 12, 2026 AT 20:38Look, if you’re gonna pop HCTZ, you better watch that potassium, okay? No one wants a heart cramp in the middle of the day. So get that banana or a supplement and keep the doc in the loop.
Kristin Violette
January 24, 2026 AT 10:25From a pharmacokinetic perspective, the prolonged half‑life of chlorthalidone (approximately 40‑60 hours) facilitates more stable plasma concentrations, thereby reducing the need for multiple daily dosing. Conversely, hydrochlorothiazide's shorter half‑life (≈6‑15 hours) may contribute to greater fluctuations in natriuresis and, consequently, blood pressure variability. The renal tubular dynamics also differ: chlorthalidone binds to the luminal side of the sodium‑chloride symporter, whereas HCTZ interacts intracellularly, which may influence downstream aldosterone signaling pathways. Clinically, these mechanistic nuances translate into observable differences in electrolyte homeostasis-specifically, the propensity for hypokalemia and secondary hyperuricemia in the HCTZ cohort. For patients with comorbid metabolic syndrome, indapamide’s combined thiazide‑like and vasodilatory actions can mitigate the adverse metabolic sequelae typically associated with traditional thiazides. Ultimately, the choice of diuretic should be predicated on a comprehensive assessment of pharmacodynamic profiles, patient-specific risk factors, and the therapeutic objectives at hand.