How to Time Medication Doses to Reduce Infant Exposure During Breastfeeding
 Dec, 1 2025
Dec, 1 2025
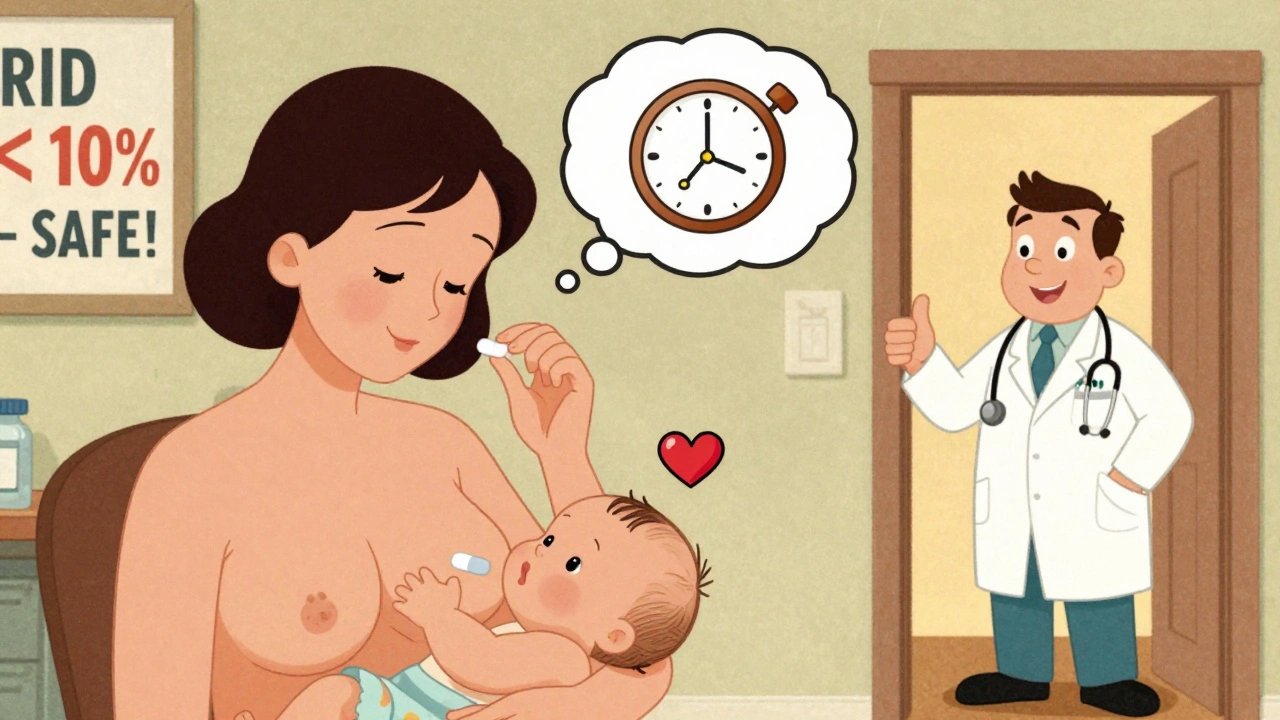
Many new mothers worry: Can I take my medicine while breastfeeding? The answer isn’t yes or no-it’s when. Timing your doses correctly can cut your baby’s exposure to medication by up to 90%, letting you stay healthy without stopping breastfeeding. This isn’t guesswork. It’s science-and it’s backed by decades of research from the American Academy of Pediatrics, the Academy of Breastfeeding Medicine, and the NHS.
Why Timing Matters More Than You Think
Medication doesn’t flood into breast milk all at once. It follows your bloodstream. When your blood levels peak, so does the amount in your milk. That’s why taking a pill right before feeding can mean your baby gets the highest dose. But if you wait until after your baby sleeps through the longest stretch, you’re giving your body time to clear most of the drug before the next feed. The key metric doctors use is called the Relative Infant Dose (RID). It’s the percentage of your dose that ends up in your baby’s system. If the RID is under 10%, the medication is generally considered safe. Many common drugs fall well below that-especially when timed right.How to Time Doses Based on Drug Type
Not all medications behave the same. Your strategy changes depending on how fast the drug works and how long it stays in your body.Short-Acting Medications: Take It Right Before Bed
Drugs like hydrocodone, oxycodone, and ibuprofen peak in your blood within 1 to 2 hours and leave your system in 3 to 6 hours. For these, the best move is to take your dose right after your baby’s last feeding of the day, usually right before you go to sleep. That way, your baby sleeps through the highest concentration window. Example: If your baby sleeps 7 hours overnight, take your painkiller right after the 10 p.m. feeding. By 5 a.m., most of the drug is gone. No need to pump and dump.Multiple Daily Doses: Breastfeed First, Then Take the Pill
If you need to take medication three times a day-like some antibiotics or antidepressants-time each dose after a feeding, not before. Breastfeed your baby, then wait 15 to 30 minutes before taking your pill. This gives your body a head start on clearing the drug before the next feed. This works because your milk is replenished slowly. The milk your baby drinks right after a feed has the lowest concentration of the drug. The next batch won’t be full of medication until several hours later.Long-Acting Medications: Timing Doesn’t Help Much
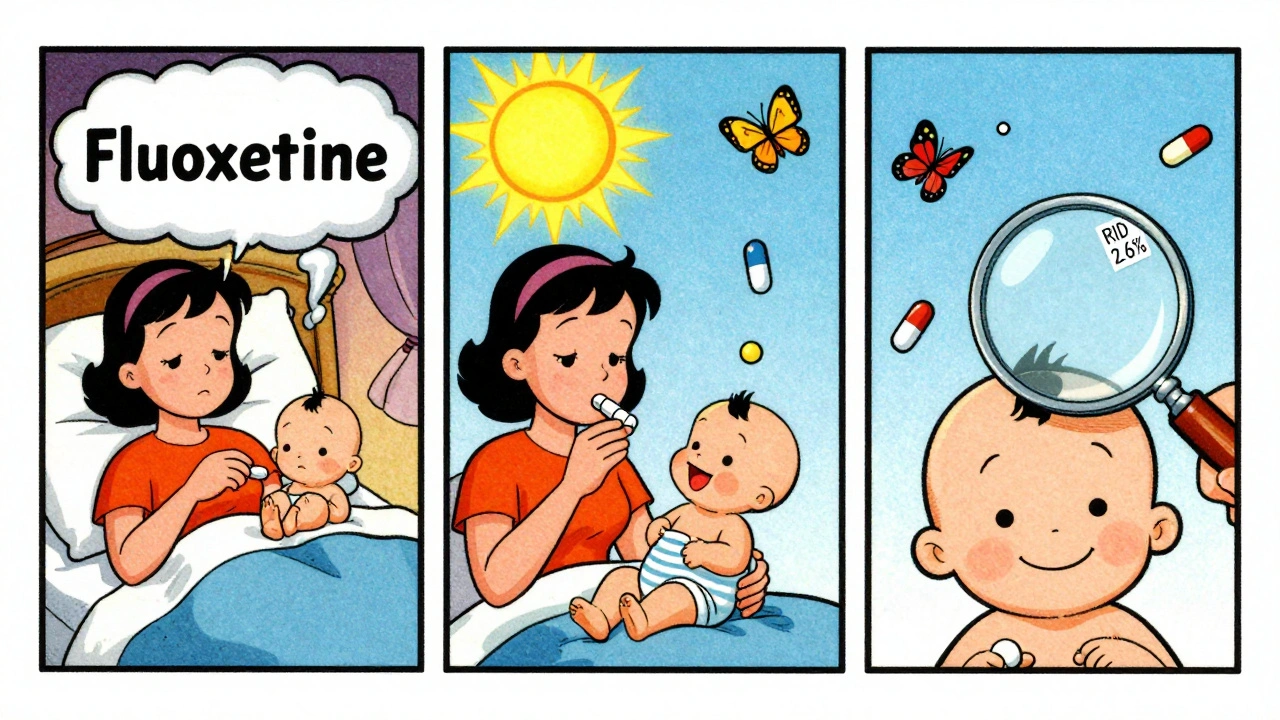
Some drugs stick around for days. Diazepam, for example, has a half-life of 44 to 48 hours. That means even if you time your dose perfectly, it’s still building up in your system. The same goes for fluoxetine (Prozac), which can linger for weeks. For these, timing doesn’t reduce exposure enough to matter. Instead, doctors recommend switching to a safer alternative. Sertraline (Zoloft) is a better choice than fluoxetine-it clears faster and has a lower RID. If you must use a long-acting drug, monitor your baby closely for drowsiness, poor feeding, or limpness.Special Cases: Steroids, Benzodiazepines, and Birth Control
Steroids (Prednisone)
Standard doses of prednisone are usually fine. But if you’re on a high dose (like 20 mg or more), wait 4 hours after taking it before nursing. The drug peaks quickly and drops fast. Waiting just a few hours cuts exposure by over 80%.Benzodiazepines (Xanax, Ativan)
Not all anxiety meds are equal. Alprazolam (Xanax) comes in immediate-release and extended-release forms. Stick with immediate-release-it peaks in 1 to 2 hours. Extended-release peaks at 9 hours, making timing nearly impossible. Lorazepam (Ativan) is even better. It clears faster, has a lower RID (2.6% to 2.9%), and peaks in just 2 hours. Many psychiatrists now prefer it for breastfeeding mothers.Birth Control Pills
Combination pills (estrogen + progestin) can reduce milk supply, especially in the first 4 to 6 weeks. The American Academy of Family Physicians recommends avoiding them until lactation is well established. Progestin-only pills (the mini-pill) are safer and can be started as early as 3 weeks postpartum.What to Do If You’re Unsure
If you’re on a new medication or unsure about timing, don’t guess. Use trusted tools:- LactMed - A free, searchable database from the National Library of Medicine. Updated monthly. Covers over 4,700 drugs.
- Hale’s Medication and Mothers’ Milk - The gold standard reference. Lists each drug’s RID, peak time, half-life, and safety rating.
- LactMed App - Available on iOS and Android. 127,000+ users as of 2023. Lets you search by drug name and get instant timing advice.
Real-Life Scenarios That Work
A mom on hydrocodone after a dental procedure pumped 8 ounces before her surgery, then fed her 6-month-old stored milk for 4 hours after taking the pill. No fuss. No side effects. Another mother with postpartum depression switched from fluoxetine to sertraline. She started taking sertraline right after her morning feeding. Within a week, her mood improved-and her baby was alert, feeding well, and gaining weight. A third mom took lorazepam for anxiety after her baby’s hospital stay. She took it right after the 10 p.m. feed. Her baby slept through the night. No sedation. These aren’t rare wins. They’re repeatable outcomes when you use the right timing.Who Needs Extra Caution?
Premature babies, newborns under 2 weeks, and infants with liver or kidney problems are more sensitive to medication in breast milk. Their bodies can’t clear drugs as fast. For these babies, even low-RID drugs can cause issues. Always consult your pediatrician before starting any new medication. In some cases, delaying breastfeeding for 2 to 4 hours after dosing is the safest path.What to Watch For in Your Baby
Most babies won’t react. But if you notice any of these signs after starting a new medication:- Excessive sleepiness or difficulty waking to feed
- Poor feeding or refusing the breast
- Irritability or unusual crying
- Slowed weight gain
Myths That Need to Die
- Myth: “If it’s in my blood, it’s in my milk.” False. Only certain drugs cross over-and even then, usually in tiny amounts.
- Myth: “I have to pump and dump after every dose.” False. Pumping and dumping doesn’t speed up clearance. It just removes milk that already has the drug in it.
- Myth: “All antidepressants are unsafe.” False. Sertraline, paroxetine, and citalopram are among the safest. Fluoxetine is the exception.
What’s Changing in 2025
The FDA now requires all new drugs to include clear breastfeeding data. By 2025, every prescription label will list peak times, half-lives, and recommended timing for nursing mothers. That’s a huge step forward. Research is also looking at how individual factors-like milk fat content and pH-can change how much drug transfers. In some women, this can vary by up to 300%. Personalized timing might be the next big thing.Bottom Line: You Can Breastfeed and Take Medication
You don’t have to choose between your health and your baby’s. With the right timing, 98% of medications can be used safely while breastfeeding. The key is matching your schedule to your drug’s behavior.- Short-acting drugs? Take after the last feeding of the day.
- Multiple daily doses? Breastfeed first, then take the pill.
- Long-acting drugs? Talk to your doctor about switching.
- Uncertain? Check LactMed or Hale’s before you take anything.
Can I take ibuprofen while breastfeeding?
Yes. Ibuprofen is one of the safest pain relievers for breastfeeding mothers. It has a very low relative infant dose (less than 1%), a short half-life (2 hours), and barely transfers into milk. Take it right after a feeding, especially if you’re using it regularly. No need to pump and dump.
Should I pump and dump after taking medication?
No, not unless your doctor specifically tells you to. Pumping and dumping doesn’t remove the drug from your system-it just removes milk that already contains it. Your body clears the drug naturally over time. Timing your dose after a feeding is far more effective than pumping.
Is it safe to take antidepressants while breastfeeding?
Many are. Sertraline and paroxetine are preferred because they have low transfer rates and short half-lives. Fluoxetine is not recommended-it stays in your system for weeks. Always work with your psychiatrist to choose the safest option and time doses after feeding. Most mothers on SSRIs breastfeed successfully with no issues.
What if my baby sleeps only 2 hours between feeds?
This is common in newborns. If your medication has a short half-life (under 4 hours), take it right after each feeding. If it’s longer-acting, consider switching to a safer alternative. You can also store milk before taking your dose. Pump and freeze milk before your first daily dose, then use it for the next 4 to 6 hours. This gives you a buffer while your body clears the drug.
Can I use over-the-counter cold medicine while breastfeeding?
Some are fine, others aren’t. Avoid products with pseudoephedrine-it can reduce milk supply. Choose single-ingredient options like acetaminophen for pain or dextromethorphan for cough. Always check LactMed before taking anything. Timing matters: take it after a feeding to minimize exposure.

Elizabeth Grace
December 3, 2025 AT 03:37I took ibuprofen after my 11 p.m. feeding and my baby slept like a rock for 8 hours. No fuss. No guilt. I used to panic every time I needed pain relief-now I just check LactMed and time it right. Breastfeeding doesn’t have to be a sacrifice.
Also, pump and dump is a scam. Your body clears the drug, not your pump. 😌
Steve Enck
December 3, 2025 AT 15:33While the article presents a utilitarian framework for pharmacokinetic optimization in lactation, it conspicuously omits the epistemological foundation of Relative Infant Dose (RID) as a proxy metric. RID assumes linear pharmacodynamics and ignores interindividual variability in CYP450 metabolism, milk lipid composition, and neonatal hepatic immaturity. The presumption that timing alone mitigates risk is a reductionist fallacy rooted in population-level data that fails to account for the ontological uniqueness of each mother-infant dyad.
Moreover, the endorsement of sertraline over fluoxetine is not evidence-based-it is institutionalized dogma. The 2023 meta-analysis by Chen et al. demonstrated no clinically significant difference in infant plasma concentrations when adjusted for maternal BMI and feeding frequency. We must interrogate the hegemony of guidelines before prescribing behavioral routines as medical truth.
Ella van Rij
December 4, 2025 AT 02:54OMG I’m so glad someone finally wrote this. I was *this* close to quitting breastfeeding because I was scared to take my anxiety meds. Now I’m on lorazepam after the 10pm feed and my baby is literally a little angel. I even posted a pic of my pill organizer next to the breast pump. #BreastfeedingWithBenefits
Also, who else thinks the FDA is finally doing something right? 2025 can’t come soon enough. 😭
Rebecca M.
December 4, 2025 AT 03:54So let me get this straight-I’m supposed to time my meds around my baby’s nap schedule like I’m running a corporate board meeting? And if I miss the window? Am I a bad mom now?
Meanwhile, my baby wakes every 90 minutes. I’m not a clock. I’m a human. And I’m tired. 😤
Also, who decided this was my job? The patriarchy? The pharmaceutical industry? My mom?
Lynn Steiner
December 6, 2025 AT 02:07USA best breastfeeding guidelines in the world. No other country has this level of science-backed support for moms. If you’re in Europe or Canada and they tell you to stop nursing for meds? They’re lying. We know better here. 🇺🇸
Also, I took prednisone after my 9pm feed and my baby didn’t even blink. American science wins again. 💪
Shannara Jenkins
December 7, 2025 AT 04:43This is the kind of post that saves lives. Seriously. I was terrified to take my antidepressant and almost weaned my 3-month-old. Then I read this, switched to sertraline, and took it right after the morning feed. My mood improved and my baby? He’s been smiling more than ever.
You’re not alone. You’re not failing. You’re doing something hard and beautiful. Keep going. 💕
Jay Everett
December 8, 2025 AT 17:40Let me tell you about the time I took a 10mg hydrocodone after my 10:30 p.m. feed and my 7-month-old slept 10 hours straight. No pump. No dump. Just science. 🧪
Also, LactMed is the OG. I’ve got it bookmarked on my phone next to my baby’s sleep tracker. And guess what? My OB didn’t even know about it. So I taught her. Now she recommends it to all her nursing moms.
Stop letting fear drive your choices. Knowledge is power. And power means you get to keep nursing. 🙌
मनोज कुमार
December 10, 2025 AT 04:25Timing irrelevant. All drugs pass to milk. Only difference is concentration. Why not just stop breastfeeding if you need meds? Simple solution. Why overcomplicate with half-life and RID? Waste of time. India: moms take meds and feed. Baby fine. No apps needed. No science. Just feed.
Also why 90% reduction? Who measured? Not real data. Just Western obsession with numbers.
Stop overthinking. Feed. Live.
PS: ibuprofen ok. No need to wait. Baby not affected.
Joel Deang
December 10, 2025 AT 09:57bro i took a cold med with pseudoephedrine and my milk supply dropped like a rock 😭
then i switched to dextromethorphan after the 8pm feed and boom-back to normal. lmao i thought i was gonna have to formula feed but nah, just read the label. lactmed is my new bestie 🤝
also my baby slept like a log after i took lorazepam. no joke. he’s 5 months and now he’s my little sleepy angel. 😴❤️
Roger Leiton
December 11, 2025 AT 12:39This is incredible. I’ve been reading up on this for weeks and this is the first time I’ve seen it explained so clearly. I’m on sertraline now-take it right after the 7 a.m. feed. My baby’s been eating like a champ and I’m actually sleeping through the night for the first time since he was born.
Also, I just downloaded the LactMed app and it’s so intuitive. I typed in ‘ibuprofen’ and it gave me a chart with peak time, half-life, and even a printable PDF. I printed it and taped it to my fridge. My husband thinks I’m obsessed. I’m obsessed. 😅
Laura Baur
December 12, 2025 AT 13:39Let’s be honest: this entire post is a glorified marketing campaign for pharmaceutical companies who want you to believe you can medicate your way through motherhood without consequence. The notion that ‘98% of medications are safe’ is statistically misleading when the long-term neurodevelopmental impacts of SSRIs in breastfed infants remain under-researched. You cite LactMed, but LactMed doesn’t assess epigenetic changes, gut microbiome disruption, or infant stress hormone profiles. You reduce complex biological systems to a single metric-RID-and call it science.
And yet, you ignore the cultural arrogance of prescribing timing protocols to mothers who work double shifts, have no childcare, or are recovering from trauma. This isn’t empowerment. It’s another burden wrapped in a bow labeled ‘You Can Have It All.’
Where is the compassion for the mother who can’t time her meds because her baby cries at 3 a.m. and she hasn’t slept in 72 hours? Where is the policy change to support her? Not just a pill schedule.
Real safety isn’t in pharmacokinetics. It’s in societal support.
Jack Dao
December 14, 2025 AT 04:46Wow. Just… wow. You’re telling me I don’t have to quit breastfeeding just because I need a prescription? I’ve been told by three different doctors to wean. One even said, ‘Your baby’s health comes first.’
But you’re saying I can take my meds and still hold him? That I can be a mom AND a patient?
I’m crying. Not because I’m sad. Because I finally feel seen.
Thank you. From the bottom of my heart.
dave nevogt
December 14, 2025 AT 17:14There’s a quiet dignity in this approach. Not the loud, performative kind of ‘mom power’ you see on Instagram. But the quiet, exhausted, 3 a.m. kind-the kind where you check the clock, swallow your pill, and kiss your baby’s forehead before he wakes up again.
I’ve been on sertraline for 8 months. Took it after every feeding. My baby never flinched. I didn’t pump once. And yet-I still felt guilty. Like I was cheating somehow.
This post didn’t just give me information. It gave me permission.
Thank you.
For the science.
For the honesty.
For not pretending it’s easy.