How to Prevent Early Refills and Duplicate Therapy Mistakes in Pharmacy Practice
 Jan, 7 2026
Jan, 7 2026
Every month, pharmacists face the same frustrating pattern: a patient walks in two weeks early for a 30-day supply of oxycodone, claiming their insurance allows it. Another comes in with a new script for gabapentin-same dose, same pharmacy-just days after their last fill. These aren’t just inconveniences. They’re red flags for duplicate therapy and dangerous early refills that can lead to overdose, addiction, or fatal drug interactions.
It’s easy to assume that if a patient got a medication before, they’re fine getting it again. But that’s exactly the mindset that gets people hurt. According to the American Academy of Family Physicians, treating refill requests as emergencies instead of predictable events leads to delays, errors, and broken trust. The CDC and Pharmacy Times both confirm: repeated early refills from multiple prescribers or pharmacies are classic signs of misuse. And with controlled substances like Schedule II opioids, DEA rules don’t even allow refills-ever.
Know the Rules: What’s Allowed and What’s Not
Not all medications have the same refill rules. The difference between a nasal steroid and an opioid isn’t just potency-it’s legality. Schedule II drugs like oxycodone, fentanyl, and Adderall cannot be refilled under any circumstances, not even by a pharmacist’s discretion. A 30-day supply means exactly 30 days. No exceptions unless the patient has a documented emergency and a new prescription from their prescriber.
For other medications, insurance policies create confusion. Most allow a 30-day script to be filled up to five days early. But patients often misinterpret that as permission to use up the medication five days early and then refill. That’s not how it works. The five-day window is for scheduling convenience, not consumption. If someone’s running out of their blood pressure pill on day 25, they shouldn’t be getting a new one until day 25-unless they’ve been seen by their provider and the refill is clinically justified.
Some health plans, like SHPNC Medicare Retirees Base PPO Plan 7030, explicitly cap early refills at 30 days total. That means if you’ve already dispensed 15 days’ worth, you can’t give more than 15 more, even if it’s “early.” This prevents stockpiling and reduces diversion risk.
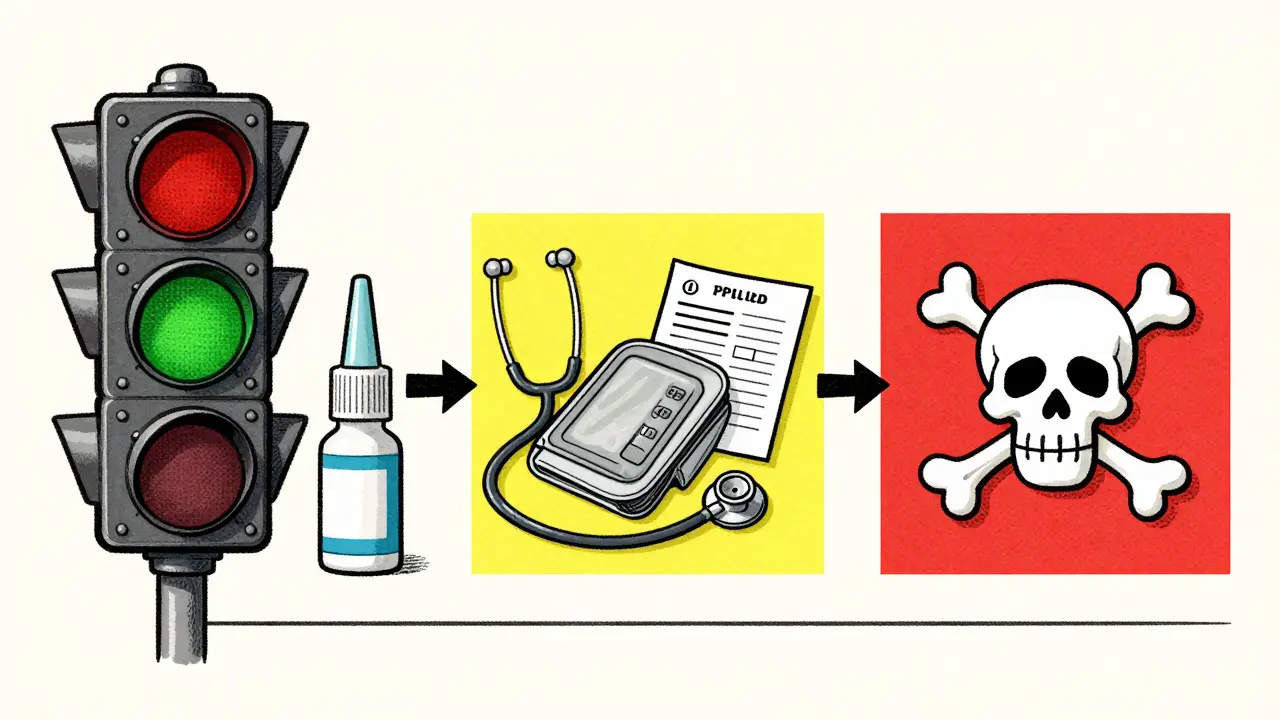
Build a Risk-Based Refill Protocol
Randomly approving refills is how mistakes happen. The best pharmacies don’t wing it-they have clear, written protocols categorized by risk level. Think of it like a traffic light system:
- Green (Low Risk): Medications like nasal steroids, thyroid hormones, or most antidepressants. These can be refilled automatically if the patient has had a visit within the last 3-6 months. No provider call needed.
- Yellow (Moderate Risk): Antihypertensives, diabetes meds, statins. These need a recent visit (within 3 months) and stable lab results. If the patient hasn’t had a blood test in 6 months, the refill is paused until they do.
- Red (High Risk): Opioids, benzodiazepines, stimulants. These require direct provider approval every time. No exceptions. Even if the patient says, “My doctor said I could get it early,” you still call the office. And if they’re getting the same drug from two different doctors? That’s a red flag.
One health system found that 89% of their refill protocols needed updating to match current guidelines. They didn’t just change the rules-they built them around evidence. For example, birth control pills got their own worksheet because they’re taken daily and refilled monthly. That’s predictable. So they pre-signed prescriptions for providers who travel, so patients never wait.
Use Technology to Catch Duplicates
Patients who see multiple doctors or use multiple pharmacies are the hardest to track. That’s why clinical viewers and prescription drug monitoring programs (PDMPs) aren’t optional-they’re essential.
Pharmacists in New Zealand and the U.S. now use tools like the Clinical Viewer to see prescriptions filled through public drug programs. If a patient walks in with a new script for tramadol, but their profile shows another fill at a different pharmacy last week, you see it before you dispense. You don’t assume they forgot. You ask: “Did your other provider know you’re taking this?”
Electronic Health Records (EHRs) help too. Providers should add notes like “Canceled prior refill” or “Prescription picked up early this month” to stop automated reminders from triggering. If your system doesn’t let you do that, push for an upgrade. Technology that flags duplicate therapy in real time reduces errors by up to 40%, according to research published in PMC.
Train Your Team to Ask the Right Questions
Front-line staff-pharmacy techs, assistants, even receptionists-are your first line of defense. They need training not just on rules, but on how to talk to patients without sounding accusatory.
Instead of saying, “You just got this last week,” try: “I see you filled this recently. Are you still having the same symptoms?” That opens the door for honest conversation. Patients might say they lost their pills, ran out early due to travel, or didn’t understand the dosage. Sometimes it’s an honest mistake. Other times, it’s the start of a pattern.
Pharmacists should also check for gaps in refill timing. If someone gets a 30-day supply on the 1st, then again on the 15th, that’s a red flag. If they come in every 20 days for the same drug, that’s not compliance-that’s misuse. Document it. Flag it. Report it if needed.
Don’t Assume Past Use Means Safe Use
Dr. Ian Stewart, a respected pharmacist and educator, put it plainly: “It cannot be assumed that since the patient has taken the medication previously, a therapeutic assessment is unnecessary.” That’s the core mistake. Just because someone took hydrocodone last year doesn’t mean they’re still safe on it now. Their liver function may have changed. They may have started a new antidepressant. Their pain may be psychological now, not physical.
Every refill is a new clinical decision. You’re not just dispensing pills-you’re evaluating risk. That means checking for:
- New medications that interact with the refill
- Changes in kidney or liver function
- Recent ER visits or hospitalizations
- Multiple prescribers or pharmacies
- Early refill patterns over time
If any of these are present, pause. Talk to the prescriber. Don’t let the patient walk out with a script until you’re sure it’s safe.
Plan for Predictable Refills
Here’s a secret: most patients who need monthly refills are predictable. They come on the same day, every month. Why treat them like emergencies?
Some practices now sign prescriptions in advance for patients on stable regimens. If Dr. Lee knows she’s going on vacation in two weeks, she signs all her patients’ refills for the next month before she leaves. That way, no one waits 24 hours for a call-back. No one ends up in the ER because they ran out of albuterol.
It’s not just about convenience-it’s about safety. When refills are planned, there’s less pressure to approve them on the spot. Staff have time to check the system. Providers have time to review. Patients get their meds on time, without drama.
What to Do When a Patient Pushes Back
Some patients will get angry. They’ll say: “My insurance says I can get it early.” “I paid cash, so you can’t stop me.” “My doctor already approved it.”
Stay calm. Say: “I understand you’re frustrated. I want to help you stay safe. Let me check with your provider to make sure this is the right next step.”
Never let guilt or pressure override protocol. If a patient threatens to go elsewhere, that’s a red flag too. Legitimate patients don’t shop for pharmacies that will ignore safety rules. They want to be cared for, not enabled.
For suspected misuse, document everything. Contact the prescriber. Consider reporting to the PDMP if your jurisdiction allows it. And if the patient has a substance use disorder, offer resources-not judgment. Recovery starts with connection, not denial.
Final Thought: Safety Isn’t Optional
Early refills and duplicate therapy aren’t just administrative headaches. They’re preventable medical errors with real consequences. One wrong refill can lead to respiratory depression. Two overlapping antidepressants can cause serotonin syndrome. A patient who gets too much opioid may not make it home.
The solution isn’t more rules. It’s better systems. Clear protocols. Trained staff. Smart tech. And the courage to say no when someone’s health is at stake.
Every time you pause a refill to check for safety, you’re not slowing things down-you’re saving lives.

Prakash Sharma
January 8, 2026 AT 00:09Man, this is why India’s healthcare is a mess-pharmacists here just hand out pills like candy. No checks, no PDMP, no damn protocol. You think this is unique to the US? Nah. We’ve got people walking into pharmacies with 5 different scripts for oxycodone and no one bats an eye. Someone needs to start enforcing rules-or people will keep dying.
Donny Airlangga
January 8, 2026 AT 10:38I’ve seen this happen in rural clinics-patients come in crying because their pain meds ran out early, and the pharmacist just gives them more to keep them quiet. It’s not malice, it’s burnout. We need systems that support pharmacists, not make them the bad guys. This post nails it: safety isn’t optional. It’s the job.
swati Thounaojam
January 9, 2026 AT 05:53my grandma got her blood pressure med early last week and the tech just gave it to her. no questions asked. kinda scary.
Aubrey Mallory
January 9, 2026 AT 15:38Let’s be real-pharmacists are the last line of defense against opioid abuse, and most are underpaid, overworked, and given zero training. You want them to catch duplicate therapy? Pay them enough to care. Give them time to check PDMPs. Stop blaming them for systemic failure. This protocol? Brilliant. But it’s useless if no one has the bandwidth to follow it.
Dave Old-Wolf
January 11, 2026 AT 09:27So if someone gets a 30-day script on the 1st, and comes back on the 15th, that’s a red flag? What if they lost it? What if their kid spilled it? What if they’re traveling and ran out early? Isn’t that being too rigid? I get the risk, but people aren’t robots. Maybe we need more compassion and fewer rules.
Molly Silvernale
January 12, 2026 AT 14:24Every pill is a story-sometimes it’s a story of chronic pain, sometimes it’s a story of desperation, sometimes it’s a story of someone who just doesn’t know how to ask for help… and we’re the ones holding the keys. We don’t just count tablets-we weigh souls. And if we’re too scared to say ‘no,’ then we’re not healers-we’re accomplices. This isn’t about policy. It’s about conscience.
Ken Porter
January 14, 2026 AT 03:22This is why America’s healthcare is broken. Over-regulated for the innocent, ignored for the addicts. Just let people buy what they want. If they OD, that’s their problem. Stop turning pharmacists into cops.
Annette Robinson
January 15, 2026 AT 12:36I love how this breaks it down into green/yellow/red. My cousin’s a pharmacy tech and she told me they just wing it most days. This would’ve saved her so much stress. Maybe we should make this part of pharmacy school curriculum? Like, mandatory. Everyone deserves to know how to spot danger before it’s too late.
Manish Kumar
January 16, 2026 AT 07:22You know, the real issue here isn’t the refills-it’s the metaphysical void that drives people to seek chemical solace. We live in a society that commodifies relief, then punishes those who reach for it. The pharmacist isn’t the gatekeeper of pills-they’re the gatekeeper of human suffering. And if we don’t fix the root-loneliness, economic despair, trauma-we’re just rearranging deck chairs on the Titanic while the opioid tide rises.
Kristina Felixita
January 16, 2026 AT 09:25oh my gosh yes!! i work at a clinic and we had this one guy come in 3 times in 2 weeks for gabapentin… i asked him gently if he was having trouble sleeping and he started crying-he said his mom passed and he couldn’t stop thinking about her. we got him connected to counseling instead of refilling. sometimes people just need someone to ask… not say no.
Joanna Brancewicz
January 16, 2026 AT 19:17PDMP integration with EHRs reduces polypharmacy errors by 40%-per PMC study. Need real-time alerts, not manual checks. Also, automated triggers for early refills should flag concurrent CNS depressants. Clinical decision support > human memory.