How to Interpret Beyond-Use Dates for Compounded Medications
 Nov, 29 2025
Nov, 29 2025
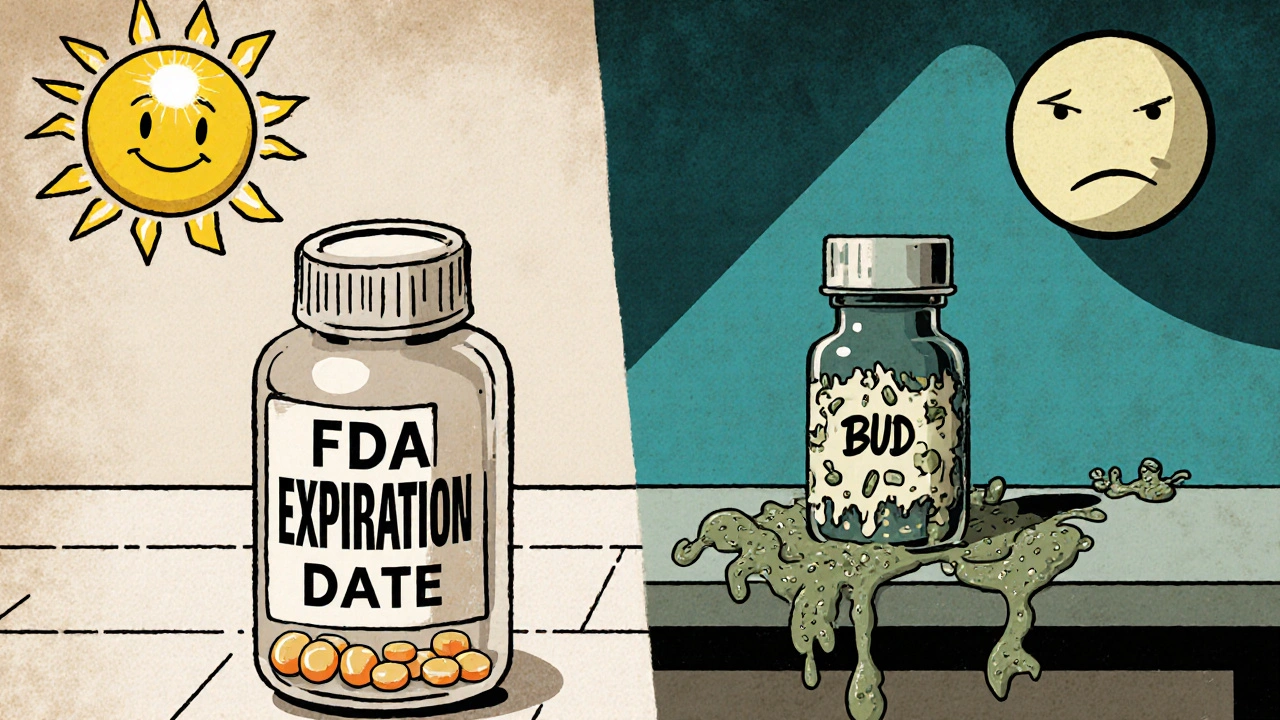
When a pharmacist hands you a vial of compounded medication, it doesn’t come with a shiny FDA expiration date like the pills you get at a chain pharmacy. Instead, it has a beyond-use date-a simple label that says, "Don’t use after this date." But what does that really mean? And why can’t you just treat it like a regular prescription? Misunderstanding this date isn’t just a paperwork error. It’s a direct risk to your health.
What Exactly Is a Beyond-Use Date?
A beyond-use date (BUD) is the last day a compounded medication is considered safe and effective to use. It’s not a guess. It’s not a suggestion. It’s a scientifically determined cutoff based on how that specific mixture will hold up over time. Unlike FDA-approved drugs, which go through years of stability testing before hitting shelves, compounded medications are custom-made. They’re mixed in small batches for individual patients-maybe a child who can’t swallow pills, someone allergic to a filler, or a patient needing a unique strength. Because they’re not mass-produced, they don’t get the same safety guarantees. That’s why the BUD exists: to fill that gap.The rules come from the United States Pharmacopeia (USP) Chapter <797>, which sets the national standard for sterile compounding. The FDA requires pharmacies to follow these rules. If a pharmacy ignores them, they’re breaking federal law. The BUD isn’t just about potency-it’s about safety. A medication can lose strength, break down into harmful chemicals, or grow dangerous bacteria. All of that can happen before the date on the label.
BUD vs. Expiration Date: The Critical Difference
It’s easy to confuse a BUD with an expiration date. They look similar. But they’re worlds apart.Expiration dates on commercial drugs are based on rigorous, FDA-mandated testing. Manufacturers test the same formula, in the same container, under controlled conditions for months or years. They measure how the active ingredient holds up, how excipients interact, and whether microbial growth occurs. Those tests are validated, repeatable, and approved by regulators.
Compounded medications? No such luck. A pharmacist has to estimate stability using four methods: manufacturer data, published studies, lab testing, or expert consultation. But here’s the catch-most of those sources don’t match the exact formula you’re holding. Maybe the study used a different solvent. Maybe the container is plastic instead of glass. Maybe the concentration is higher. Even small changes can make a huge difference. A 2021 study found that changing the pH of a compounded solution could speed up degradation by 3.7 times compared to the commercial version.
That’s why you can’t assume a compounded liquid has the same shelf life as its tablet form. You can’t assume a syringe-stored dose lasts as long as a vial. And you absolutely can’t extend the BUD because "it still looks fine." The color, smell, or clarity of the liquid tells you nothing about its chemical safety.
How Pharmacists Determine BUDs-And Where They Go Wrong
Assigning a BUD isn’t a one-step process. It’s a five-part decision tree.- Identify all components. What’s in the mix? Active drug? Solvent? Preservatives? Even small additives like flavoring can affect stability.
- Classify the risk level. USP <797> divides compounding into low, medium, and high risk. Low-risk means minimal handling-like mixing a sterile solution in a clean room. High-risk means complex procedures, like preparing IV bags from multiple vials in a non-sterile environment. Higher risk = shorter BUD.
- Check manufacturer labels. If the original drug has an expiration date or storage instructions, that’s your starting point. The FDA says you can’t exceed those limits.
- Consult validated literature. Is there a peer-reviewed study on your exact formula? Most pharmacists struggle here. A 2023 survey found 63.8% of compounding pharmacies couldn’t find reliable data for their specific mix.
- Apply professional judgment. This is where experience matters. But it’s also where mistakes happen. A 2022 analysis showed that 68% of BUD errors came from ignoring how the container interacts with the drug. A plastic syringe might leach chemicals into the solution. A glass vial might absorb the active ingredient. Neither is safe to assume.
And here’s the scary part: only 37.2% of pharmacies use properly validated stability testing methods like HPLC. Most rely on guesswork. That’s why the FDA issued 34.1% more BUD-related warnings in 2023 than in 2022. One pharmacy recalled over 1,200 products in 2021 because bacteria grew in syringes labeled with BUDs based on vial data-something the FDA explicitly warns against.
What BUDs Actually Look Like in Practice
The maximum BUDs allowed under USP <797> depend on risk level and storage:- Low-risk, room temperature: Up to 48 hours
- Medium-risk, refrigerated: Up to 14 days (increased from 7 days in the 2023 update)
- High-risk, frozen: Up to 45 days (if stability testing confirms it)
But these are maximums. The real BUD is often much shorter. A compounded antibiotic suspension might only last 7 days, even if the guidelines allow 14. A hormone cream stored in a plastic tube might degrade in 10 days, even if the literature says 30. It all depends on the formulation.
Water-based formulas are especially tricky. They’re prone to microbial growth. The 2023 USP update raised the BUD for water-based preparations from 14 to 30 days-but only if the pharmacy has proof the formula stays sterile. Without testing, the clock still starts ticking at 14 days. And if you’re storing it in a syringe? That’s not approved for long-term storage. The FDA says so. Yet 41.3% of retail pharmacies still use syringe data to assign BUDs for other containers.
Why You Should Never Stretch a BUD
You might think, "It’s only a few days past the date. It’s probably fine." But that’s how outbreaks start.In 2022, a patient developed a bloodstream infection from a compounded steroid injection. The BUD had been extended by 11 days based on a study that didn’t match the exact formulation. The drug had degraded, and bacteria had grown. The patient spent weeks in the hospital. The pharmacy lost its license.
Stability isn’t about appearance. A cloudy solution? Yes, that’s a red flag. But a clear one? Doesn’t mean it’s safe. Degradation products can be invisible. Bacteria can multiply without changing the color. A 2023 study showed that 63% of degraded compounded drugs showed no visible signs of spoilage.
And it’s not just about infection. A pain medication that loses 20% of its potency means the patient still suffers. A hormone dose that’s too strong could cause dangerous side effects. The margin for error in compounded meds is tiny. That’s why the BUD exists-to keep you safe when science can’t guarantee perfection.

What You Can Do as a Patient
You don’t need to be a pharmacist to protect yourself. Here’s what to ask:- "What’s the BUD, and how was it determined?" If the answer is "It’s the same as the original drug," walk away. That’s not enough.
- "Is this stored in the right container?" If it’s in a syringe, ask if that’s approved for long-term storage. It usually isn’t.
- "Can I get documentation on how this date was set?" Pharmacies are required to keep written justification. Ask for it.
- "What should I do if it looks different?" Cloudiness, particles, strange odor? Don’t use it. Return it.
Don’t be shy. This isn’t a dumb question. It’s a life-saving one. If a pharmacy refuses to explain their BUD, find another one. Compounding isn’t a gray area-it’s a science. And you deserve to know the science behind your medicine.
The Future of BUDs: What’s Changing
The rules are tightening. USP’s 2024 draft proposes requiring direct stability testing for any BUD over 30 days. That could affect nearly a quarter of current compounded medications. The FDA is increasing inspections. Insurance companies are starting to audit BUD documentation.Technology is helping, too. Some pharmacies now use real-time monitoring systems that track temperature, light exposure, and even chemical stability. One pilot study showed a 47% drop in BUD errors with these tools.
As personalized medicine grows-projected to make up nearly 1 in 5 prescriptions by 2030-accurate BUDs will become even more critical. More patients will need custom formulations. More pharmacies will try to cut corners. The stakes are rising.
Bottom line: A beyond-use date isn’t just a label. It’s a promise. A promise that someone took the time to test, to verify, to protect you. Don’t let that promise be broken.

Karandeep Singh
November 29, 2025 AT 19:32Bonnie Youn
December 1, 2025 AT 08:18Debbie Naquin
December 3, 2025 AT 01:07elizabeth muzichuk
December 3, 2025 AT 08:21Charlotte Collins
December 4, 2025 AT 07:36Amber-Lynn Quinata
December 6, 2025 AT 01:44Kelly Essenpreis
December 7, 2025 AT 13:53Edward Hyde
December 9, 2025 AT 11:51ariel nicholas
December 9, 2025 AT 14:03Margaret Stearns
December 11, 2025 AT 00:00Scotia Corley
December 12, 2025 AT 02:28amit kuamr
December 13, 2025 AT 19:51Erin Nemo
December 13, 2025 AT 23:08