How to Avoid Liver Injury from OTC Pain Relievers
 Dec, 16 2025
Dec, 16 2025
Every year, thousands of people end up in the emergency room because they took too much of a common pain reliever-something they thought was completely safe. Acetaminophen, the active ingredient in Tylenol and hundreds of other OTC products, is the leading cause of acute liver failure in the United States. And most of these cases aren’t from suicide attempts. They’re from mistakes-taking one extra pill, combining cold medicine with painkillers, or thinking "a little more won’t hurt."
Why Acetaminophen Is So Dangerous
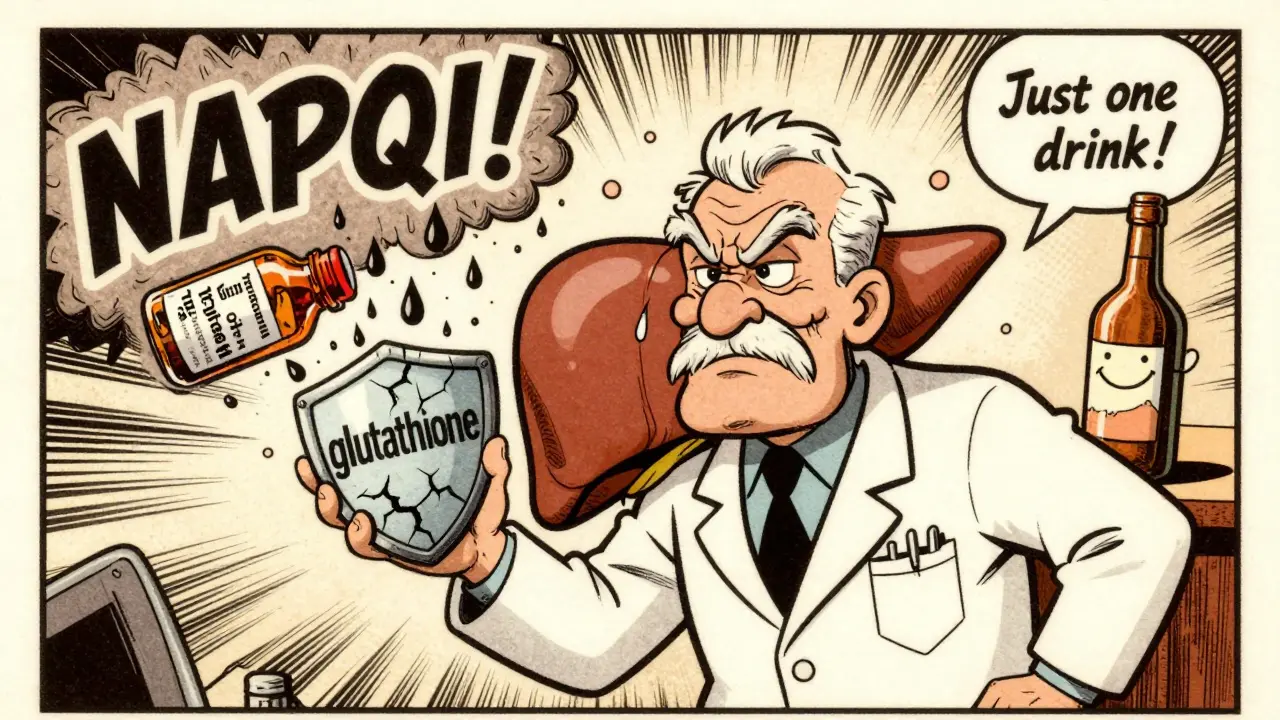
Acetaminophen works great for pain and fever. It’s in more than 600 medications, from headache tablets to nighttime sleep aids. But your liver processes it differently than other drugs. When you take it, your liver turns most of it into harmless waste. But a small portion becomes a toxic chemical called NAPQI. Normally, your liver neutralizes it with glutathione, an antioxidant. But if you take too much, your glutathione runs out. That’s when NAPQI starts killing liver cells.
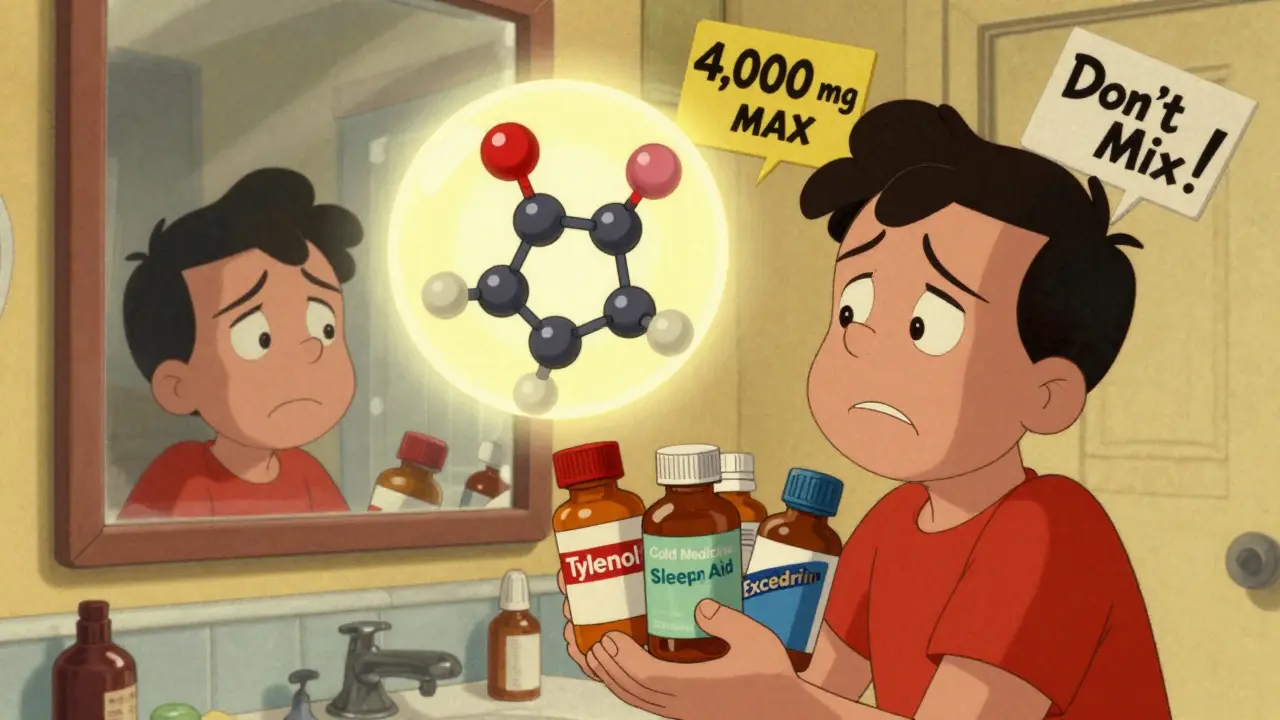
The official daily limit for healthy adults is 4,000 mg. But that number is misleading. Many people hit that limit without realizing it. One extra-strength Tylenol tablet is 500 mg. Four of them? That’s 2,000 mg. Add a cold medicine with 325 mg of acetaminophen per tablet? Now you’re at 2,325 mg-before you even take your next pain reliever. By bedtime, you could easily be over 4,000 mg without ever thinking you were overdosing.
Who’s at Highest Risk
Not everyone reacts the same way. People with existing liver disease-like fatty liver, hepatitis, or cirrhosis-have less glutathione to begin with. Their safe limit drops to 2,000 mg per day. That’s just four regular-strength pills. The Veterans Affairs Hepatitis Resource Center says these patients should avoid alcohol completely when taking acetaminophen. Alcohol and acetaminophen together can crash the toxic threshold down to 2,000 mg or even lower.
Even healthy people aren’t immune. Genetics play a role. Some people naturally produce less glutathione or process acetaminophen slower. New genetic tests, like those from 23andMe, can now identify these higher-risk individuals. If you’ve had unexplained liver enzyme spikes in the past, or if your family has a history of liver issues, you might be more vulnerable than you think.
NSAIDs Aren’t the Safe Alternative
Many people switch to ibuprofen or naproxen thinking they’re safer for the liver. But that’s not true. While NSAIDs don’t usually cause direct liver damage like acetaminophen, they carry their own dangers. Diclofenac, in particular, is linked to rare but serious liver injury. More importantly, NSAIDs can cause stomach bleeding, kidney damage, and high blood pressure. For someone with liver disease, NSAIDs can also worsen fluid retention and increase the risk of kidney failure.
The American Liver Foundation doesn’t recommend NSAIDs as a first choice for people with advanced liver conditions. Topical NSAID creams or gels are a better option-they enter the bloodstream in tiny amounts and rarely affect the liver. For chronic pain, physical therapy, acupuncture, or cognitive behavioral therapy are safer long-term solutions.
How to Avoid Accidental Overdose
Here’s the hard truth: you can’t trust the label if you don’t know what to look for. Acetaminophen hides in cold medicines, flu remedies, sleep aids, and even some prescription painkillers like Vicodin or Percocet. Always check the active ingredients list-not the brand name.
- Never take more than one acetaminophen-containing product at a time.
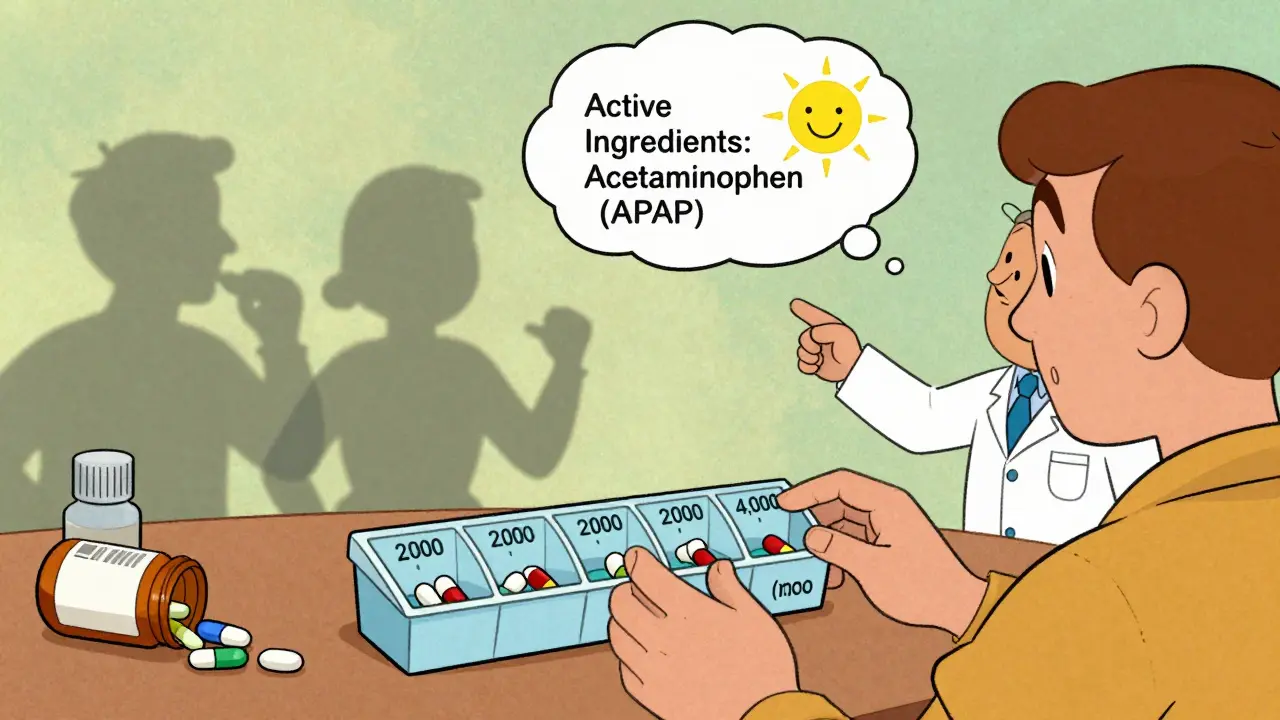
- Use a pill organizer with daily max indicators-mark 4,000 mg as your hard stop.
- Avoid alcohol entirely while taking acetaminophen.
- Keep a medication diary: write down every pill you take, including time and dose.
- Check labels on every OTC product-even if you’ve used it before. Formulas change.
According to the FDA, about 25% of unintentional overdoses happen because people don’t realize their cold medicine contains acetaminophen. That’s why the FDA now requires a prominent "Liver Warning" on the front of all OTC acetaminophen packages. Look for it.
What to Do If You Think You’ve Taken Too Much
Don’t wait for symptoms. Nausea, vomiting, loss of appetite, fatigue, and pain in the upper right side of your abdomen are signs your liver is under stress. Jaundice (yellow skin or eyes), dark urine, or clay-colored stools mean your liver is already damaged.
If you suspect an overdose-even if you’re not sure-call poison control immediately or go to the ER. The antidote, N-acetylcysteine (NAC), works best if given within 8 hours. After 16 hours, its effectiveness drops sharply. Time matters more than you think.
Even if you feel fine, get checked. Liver damage can be silent at first. Blood tests for ALT and AST enzymes can show injury before you feel sick.
What’s Changing in 2025
The FDA lowered the maximum daily dose for prescription combination products from 4,000 mg to 3,250 mg in 2021. In 2022, they mandated clearer labeling on all OTC packages. Since then, unintentional overdoses have dropped by 21%, according to Johns Hopkins University.
New research is pushing toward personalized dosing. Companies are now offering genetic tests to identify people who metabolize acetaminophen slowly. If you’re at high risk, your doctor might recommend a max of 2,000-3,000 mg per day-even if you’re healthy.
The National Institutes of Health is investing $47 million through 2028 to develop new pain relievers that don’t rely on liver metabolism. The future of pain management may be non-systemic: patches, creams, nerve blocks, and digital therapies.
Bottom Line: Take Control
Acetaminophen isn’t evil. It’s a lifesaver when used right. But it’s not harmless. It’s a tool-and like any tool, misuse can cause serious harm.
Here’s your action plan:
- Know your limit: 4,000 mg max for healthy adults, 2,000 mg if you have liver disease.
- Read every label. Every time.
- Never mix acetaminophen with alcohol.
- Use non-drug options for chronic pain first.
- When in doubt, skip it or ask your pharmacist.
Your liver doesn’t scream before it fails. It whispers. Learn to listen.
Can I take acetaminophen if I have fatty liver disease?
Yes, but only up to 2,000 mg per day. Fatty liver disease reduces your liver’s ability to process acetaminophen safely. Even at normal doses, your risk of liver injury increases. Avoid alcohol completely and track every dose. Talk to your doctor about alternatives like physical therapy or topical pain relievers.
Is Tylenol safer than ibuprofen for the liver?
For the liver, yes-acetaminophen is the preferred choice over NSAIDs like ibuprofen, but only if you stay under 4,000 mg daily. NSAIDs rarely cause liver damage directly, but they can harm your kidneys and stomach, especially if you have liver disease. The key is using the lowest effective dose of the right drug for your situation.
How do I know if a cold medicine has acetaminophen?
Look at the "Active Ingredients" section on the label. It will list "acetaminophen," "paracetamol," or the abbreviation "APAP." Common brand names include Tylenol, Excedrin, NyQuil, DayQuil, and Theraflu. Never assume a product is safe just because it’s labeled "cold and flu"-always check the ingredients.
What are the early warning signs of liver damage from pain relievers?
Early signs include nausea, vomiting, loss of appetite, fatigue, and pain in the upper right side of your abdomen. These can appear within 24 to 72 hours after an overdose. Later signs-jaundice, dark urine, pale stools-mean serious damage is already happening. Don’t wait for yellow skin. If you’ve taken too much acetaminophen and feel off, get tested.
Is it safe to take acetaminophen every day for chronic pain?
Taking acetaminophen daily for more than a few weeks increases your risk, even if you stay under 4,000 mg. The liver doesn’t get a break. For chronic pain, the American Liver Foundation recommends non-drug treatments first: physical therapy, acupuncture, or cognitive behavioral therapy. If you must use medication, work with your doctor to find the lowest effective dose and take breaks when possible.
Can I take acetaminophen after drinking alcohol?
No. Even one drink can lower your safe acetaminophen threshold. Alcohol depletes glutathione, the liver’s natural defense against the toxic byproduct of acetaminophen. This combination can cause liver injury at doses you’d normally think are safe. Wait at least 24 hours after drinking before taking acetaminophen-and even then, use caution.
Does the FDA limit how much acetaminophen is in each pill?
Yes. Since 2011, the FDA has required OTC acetaminophen products to limit each tablet or capsule to no more than 325 mg. Many manufacturers now make 500 mg or 650 mg pills, but these are labeled as "extra-strength" and must carry clear warnings. Prescription combinations (like those with opioids) are capped at 325 mg per dose. Always check the strength on the label.
What should I do if I accidentally take too much acetaminophen?
Call poison control immediately at 1-800-222-1222 or go to the nearest emergency room. Don’t wait for symptoms. The antidote, N-acetylcysteine (NAC), works best within 8 hours of ingestion. Even if you feel fine, get checked. Liver damage can be silent until it’s too late.

Joe Bartlett
December 16, 2025 AT 21:59Been taking Tylenol for years, never knew it could wreck your liver. Mind blown.
Jigar shah
December 17, 2025 AT 07:59This is one of the most well-researched pieces on OTC meds I've read. The breakdown of NAPQI and glutathione is exactly what people need to understand. Most don't realize acetaminophen is in 600+ products. I've started checking every label since reading this.
Jody Patrick
December 17, 2025 AT 14:41USA leads in liver failure from painkillers? That's what you get when you let corporations control medicine.
Kaylee Esdale
December 18, 2025 AT 15:29My grandma took Tylenol every night for her arthritis and never knew she was slowly frying her liver. She’s 82 now and her enzymes are fine because she stopped cold turkey after reading this. Thank you for saving her life without even knowing it.
Meghan O'Shaughnessy
December 18, 2025 AT 18:23As someone who grew up in a household where "a little more won’t hurt" was the motto, this hits hard. My dad ended up in the ER at 48 from mixing cold meds and painkillers. He thought he was being smart. Turns out he was just unlucky. Now I carry a little card in my wallet that says "Check the label. Always."
Philippa Skiadopoulou
December 20, 2025 AT 01:15Important to note that NSAIDs like diclofenac carry their own hepatotoxic potential, though less common than acetaminophen. The real issue is polypharmacy and lack of patient education. Pharmacists should be mandatory in OTC aisle consultations.
Marie Mee
December 21, 2025 AT 09:35They’re hiding it in everything and no one tells you. Big Pharma knows people will keep taking it because it works. They don’t care if your liver dies as long as you keep buying pills. I saw a documentary once where they admitted they lobbied against the 325mg limit. This is all planned.
Nishant Desae
December 22, 2025 AT 00:01Hey everyone, just wanted to say this post saved my life. I’ve been taking extra strength Tylenol every night for back pain for 3 years. Never thought twice about it. Then I saw the part about fatty liver and realized I had been diagnosed with it last year and forgot. I went to my doc, got tested, my ALT was sky high. Now I’m on physical therapy, using a topical cream, and only taking 500mg max if I absolutely have to. I’m 32 and didn’t want to be one of those people who woke up one day with liver failure. Thanks for the wake up call. If you’re reading this and take meds daily - check your labels. Seriously. Just stop for a second and look. You might be surprised.