Fluoroquinolone Side Effects: Tendinopathy and Nerve Damage Risks
 Dec, 6 2025
Dec, 6 2025
Fluoroquinolone Side Effect Risk Calculator
Fluoroquinolone Side Effect Risk Calculator
This tool helps you understand your personal risk of tendon damage or nerve damage when taking fluoroquinolone antibiotics like ciprofloxacin or levofloxacin. Based on your health factors, it calculates your relative risk compared to average users.
Your Risk Assessment
What This Means
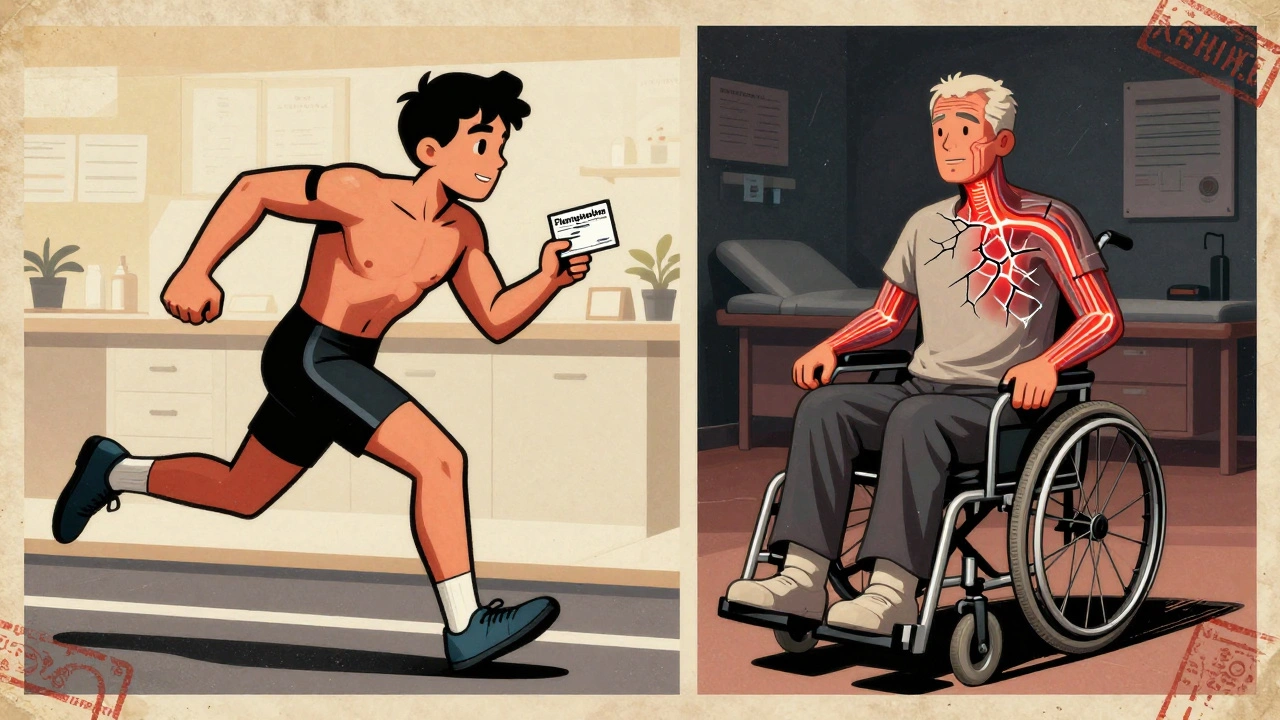
When you take an antibiotic like ciprofloxacin or levofloxacin for a sinus infection or urinary tract infection, you expect to feel better in a few days. But for some people, the relief never comes - because the drug itself starts breaking down their body. Fluoroquinolones, once hailed as miracle antibiotics, are now known to cause tendon rupture and nerve damage that can last for years - or never go away at all.
What Are Fluoroquinolones, and Why Are They Still Prescribed?
Fluoroquinolones are a class of antibiotics that include ciprofloxacin, levofloxacin, moxifloxacin, and norfloxacin. They were developed in the 1960s and became popular because they work against a wide range of bacteria, penetrate tissues deeply, and come in pill form. For serious infections like anthrax, hospital-acquired pneumonia, or complicated kidney infections, they can still be life-saving. But here’s the problem: for most common infections - like a simple bladder infection, sinusitis, or bronchitis - they’re not necessary. And the risks? They’re not small. The U.S. Food and Drug Administration (FDA) issued a black-box warning in 2008, then strengthened it in 2016 after reviewing thousands of reports. Their message was clear: only use fluoroquinolones when no other antibiotic will work.Tendon Damage: More Common Than You Think
Tendons connect muscle to bone. They’re tough, but they’re not invincible. Fluoroquinolones weaken them. The Achilles tendon - the thick band at the back of your ankle - is the most commonly affected, making up nearly 90% of cases. But shoulders, hands, and thumbs can also rupture. The numbers don’t lie:- Between 0.14% and 0.4% of people taking fluoroquinolones develop tendinopathy.
- Up to 40% of those cases end in full tendon rupture.
- Half of all tendon injuries happen after you’ve stopped taking the drug - sometimes weeks or even months later.
Nerve Damage: A Silent, Lasting Threat
Peripheral neuropathy is another devastating side effect. It’s not just numbness or tingling - it’s burning, electric shocks, loss of balance, and muscle weakness. In some cases, it’s permanent. Studies show:- 4.3% of patients on fluoroquinolones develop peripheral neuropathy.
- Onset can happen within days - even before finishing the course.
- Up to 10% of patients report long-term disability: trouble walking, loss of fine motor skills, chronic pain.
Who’s Most at Risk?
Not everyone gets hurt. But certain people are far more vulnerable:- Age 60+: 1.5 times higher risk of tendinopathy, 2.7 times higher risk of rupture.
- On corticosteroids: 46 times higher risk of tendon rupture.
- Diabetes or kidney disease: Increased risk of both tendon and nerve damage.
- History of tendon problems: If you’ve had a prior rupture, don’t take these drugs.
- High-intensity athletes: Even young, healthy people can rupture tendons under stress.
What Should You Do If You’re Prescribed One?
Don’t panic. But do ask questions.- Ask: “Is this infection serious enough to justify fluoroquinolones?”
- Ask: “Are there safer alternatives like amoxicillin, doxycycline, or trimethoprim-sulfamethoxazole?”
- Ask: “What are the signs of tendon or nerve damage - and what should I do if I feel them?”
- Stop immediately if you feel pain, swelling, or tingling in your tendons or nerves.
- Don’t wait for a doctor’s appointment - get off the drug now.
- Never take steroids while on fluoroquinolones.
- Rest the affected area. Ice it. Avoid exercise.
Why Are These Drugs Still on the Market?
Because they work - for the right cases. In hospitals, for drug-resistant infections, or for bioterror threats like anthrax, fluoroquinolones still have value. But for 90% of the time they’re prescribed - for sinus infections, UTIs, or bronchitis - they’re not needed. Since the FDA and EMA tightened restrictions in 2016-2019, prescribing for minor infections has dropped by over 70%. In the U.S., fluoroquinolone use for UTIs fell from 17.3% in 2015 to just 5.1% in 2022. The global market for these drugs has shrunk by 27% since 2015. The problem isn’t the drugs themselves - it’s how often they’re misused.What’s Being Done Now?
Regulators are paying attention:- The FDA’s Sentinel Initiative now tracks real-time adverse events across 150 million Americans.
- The European Medicines Agency confirmed the 4.1-fold increased risk of Achilles rupture in a 2023 study.
- New clinical trials are testing whether doxycycline can protect tendons during fluoroquinolone treatment.
- Three new antibiotics are in late-stage trials, aiming to replace fluoroquinolones by 2026-2028.
Real Stories, Real Damage
The Fluoroquinolone Effects Research Foundation has collected over 8,500 patient reports. 78% had tendon issues. Median symptom duration? 14 months. In Australia’s Floxie support group, 35% of members needed surgery. On Drugs.com, ciprofloxacin has a 2.2/5 rating - and 68% of negative reviews mention tendon or nerve damage. One woman in her 50s took ciprofloxacin for a UTI. Three weeks later, her Achilles tendon snapped while walking. She couldn’t walk for six months. Her doctor said, “It’s just age.” She later found out it was the antibiotic. Another man, 68, took levofloxacin for bronchitis. Two weeks after finishing, his hands went numb. He couldn’t button his shirt. His neurologist said it was carpal tunnel. It wasn’t. It was permanent nerve damage. These aren’t rare outliers. They’re the rule.Bottom Line: Don’t Take Fluoroquinolones Unless You Have To
Fluoroquinolones are not harmless. They’re powerful drugs with dangerous, long-lasting side effects. Tendon rupture and nerve damage aren’t just risks - they’re well-documented outcomes. If you have a mild infection, there are safer options. Ask for them. Push back if your doctor pushes fluoroquinolones. If you’re already on one and feel pain or tingling - stop immediately. Don’t wait. Don’t hope it goes away. Document everything. Get help. Your tendons and nerves don’t regenerate easily. Once they’re damaged, recovery is uncertain - and often incomplete.Frequently Asked Questions
Can fluoroquinolone tendon damage be reversed?
In some cases, yes - if caught early and the drug is stopped immediately. But many patients experience permanent damage. Tendon rupture often requires surgery and months of rehab. Nerve damage can be irreversible, with chronic pain, numbness, or weakness lasting years. Up to 10% of patients report long-term disability.
How long after stopping the drug can side effects start?
Symptoms can appear as early as the first day of treatment - or as late as 152 days after stopping. Half of all tendon injuries occur after the patient has finished the course. Nerve damage can show up weeks later. This delay is why many people don’t connect their symptoms to the antibiotic.
Are all fluoroquinolones equally dangerous?
Ciprofloxacin is the most commonly reported cause of tendon damage, followed by levofloxacin and moxifloxacin. But all fluoroquinolones carry the same black-box warnings. No one is safer than another when it comes to tendon or nerve risks.
Can I take fluoroquinolones if I’m young and healthy?
Even young, healthy people can suffer tendon rupture or nerve damage. Athletes, runners, and weightlifters are at higher risk due to physical stress on tendons. The drug doesn’t discriminate by age - it targets collagen and nerve cells. If there’s a safer alternative, use it.
What should I do if I think I’m having side effects?
Stop taking the drug immediately. Rest the affected area. Avoid stretching or exercise. Contact your doctor and mention fluoroquinolone toxicity. Bring documentation - including this article. If you have pain in a tendon or tingling/numbness in your limbs, don’t wait. Early action improves outcomes.
Are there safer antibiotics for UTIs or sinus infections?
Yes. For uncomplicated UTIs, nitrofurantoin, trimethoprim-sulfamethoxazole, or fosfomycin are preferred. For sinus infections, amoxicillin or doxycycline are first-line. Fluoroquinolones should only be used if these fail or if you’re allergic. Most doctors still overprescribe fluoroquinolones - so ask for alternatives.

David Brooks
December 8, 2025 AT 04:40Bro, I took cipro for a UTI back in 2019 and thought I was fine until I couldn’t walk one morning. My Achilles just *snapped* like a rubber band. No trauma, no fall. Just… gone. Took 14 months to walk normally again. Now I tell every person I know: if your doc pushes fluoroquinolones, ask for amoxicillin instead. Your tendons will thank you. 🙏
Jennifer Anderson
December 9, 2025 AT 10:27ok so i just got prescribed levaquin for a ‘bad’ sinus infection and i was like ‘ehh maybe’ but then i read this and i’m like… NOPE. i called my dr and asked for amoxicillin. she was like ‘well cipro is stronger’ and i said ‘but i’d rather be weak than paralyzed.’ she gave me the amox. y’all. protect yourselves. 🙌
Sadie Nastor
December 9, 2025 AT 23:10thank you for writing this. i’ve been silent about my nerve damage for years because no one believed me. ‘it’s just aging’ they said. ‘carpal tunnel’ they said. turns out it was moxifloxacin. i still get electric shocks in my fingers when it’s cold. i’m not ‘overdramatic’-i’m just surviving. if you’re reading this and you’re on one of these drugs? stop. now. and tell someone. you’re not alone. 💙
Nicholas Heer
December 11, 2025 AT 20:10THIS IS A PHARMA COVER-UP. The FDA knew. The WHO knew. They let Big Pharma push these drugs because they’re profitable. Look at the timeline-2008 warning, 2016 strengthened, but prescriptions kept climbing until 2020. Coincidence? Nah. The same companies that made Vioxx and OxyContin are behind this. They don’t care if you lose your mobility-they care about quarterly earnings. Wake up. This is systemic evil.
Sangram Lavte
December 13, 2025 AT 02:56In India, doctors still prescribe cipro like candy for diarrhea or sore throat. No one talks about side effects. My uncle got tendon rupture after a simple bronchitis course. He’s 62, diabetic, on steroids. They didn’t even mention the risks. This needs global awareness. Not just US/EU.
Oliver Damon
December 14, 2025 AT 16:14There’s a deeper philosophical question here: when does medical progress become medical hubris? We developed these drugs to conquer infection, but we forgot that the human body isn’t a machine to be optimized-it’s an ecosystem. Fluoroquinolones don’t just kill bacteria; they disrupt collagen synthesis, mitochondrial function, and neuronal integrity. We treated symptoms without understanding mechanisms. And now we’re paying the price. It’s not just about antibiotics-it’s about humility in medicine.
Kurt Russell
December 16, 2025 AT 04:42IF YOU’RE ON FLUOROQUINOLONES AND YOU FEEL ANYTHING-TINGLING, STIFFNESS, PAIN-STOP. NOW. I’M NOT JOKING. I’VE SEEN TOO MANY PEOPLE WAIT. THEY THINK IT’LL PASS. IT WON’T. I GOT MY KNEE TENDON REPAIRED AFTER 8 MONTHS OF PAIN. I’M STILL IN PHYSICAL THERAPY. DON’T BE A STATISTIC. ASK FOR ALTERNATIVES. BE YOUR OWN ADVOCATE. YOU GOT THIS.
Stacy here
December 16, 2025 AT 23:34Let’s be real-doctors are overworked and underpaid. They don’t have time to read the 50-page FDA warning. They grab the easiest script: cipro. It’s not malice, it’s systemic burnout. But that doesn’t excuse the outcome. We need better education, not just warnings. And patients? We need to stop being passive. If your doctor says ‘it’s fine,’ say ‘prove it.’ Show them this post. Make them earn your trust.
Kyle Flores
December 17, 2025 AT 07:11My mom took levofloxacin for a UTI and got nerve damage in her feet. She couldn’t feel her toes for 2 years. The doctor said it was ‘unlikely.’ Turns out it was the drug. I showed him the FDA warning. He apologized. But no one else ever will. That’s why we share stories like this. So the next person doesn’t get ghosted by the system.
Ryan Sullivan
December 18, 2025 AT 14:56Pathetic. People whine about side effects like they’re entitled to zero risk. Antibiotics are inherently dangerous. You want safety? Don’t get infected. If you can’t handle the collateral damage of modern medicine, maybe don’t live in a post-industrial society. This isn’t a conspiracy-it’s biology. Stop crying and take responsibility.
Wesley Phillips
December 19, 2025 AT 20:37Look I’m not saying this isn’t real but like… cipro is basically the Kool-Aid of antibiotics. Everyone’s just like ‘oh yeah I took it once’ like it’s a meme. Meanwhile I’m over here with a 30% chance of tendon rupture and my neurologist still thinks I’m exaggerating. Just… stop. Just stop. I’m not mad. I’m just… done.