Drug Withdrawals and Recalls: Why Medications Get Removed from Market
 Oct, 31 2025
Oct, 31 2025
Drug Withdrawal Timeline Simulator
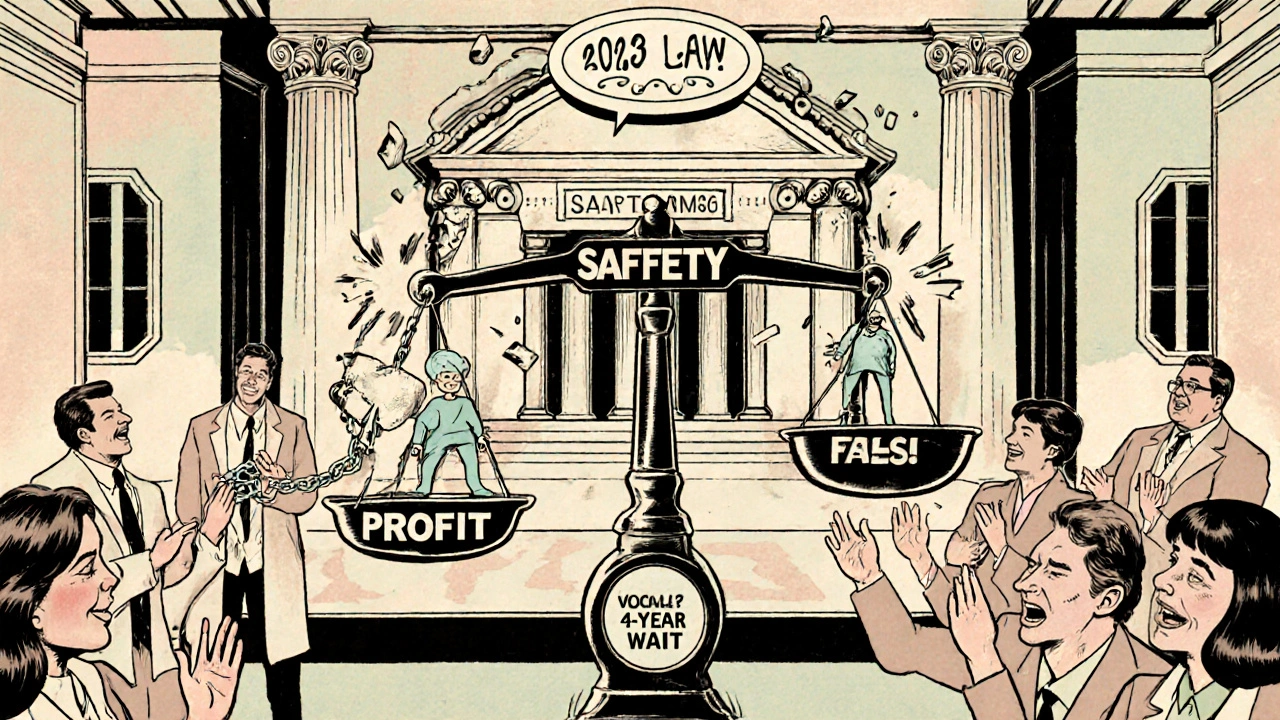
How Drug Withdrawals Work: Old vs New System
The FDA's process for removing ineffective or unsafe drugs changed dramatically in 2023. See how it differs between the old system and the new law.
Old System (Pre-2023)
Up to 46 months average
Often takes years to run required follow-up studies
No clear deadlines for companies to submit follow-up studies
Average 46 months from study completion to withdrawal decision
Companies could appeal decisions, causing further delays
New System (Post-2023)
Max 180 days
Must prove drug is ineffective or unsafe
FDA must notify company within 30 days of proposing withdrawal
Company gets meeting with FDA leadership within 60 days
Final decision must come within 180 days
Real-World Impact
Old System Impact
Up to $8 billion wasted on ineffective drugs between 2010-2020
26% of accelerated approval drugs eventually withdrawn
41% of eligible small cell lung cancer patients continued receiving ineffective drugs
New System Impact
First drug pulled in <6 months (ALS treatment)
FDA now uses real-world data to monitor drug effectiveness
Potential to identify issues 18 months faster than traditional studies
Every year, dozens of medications disappear from pharmacy shelves-not because they’re outdated, but because they’re dangerous or don’t work. These aren’t rare mistakes. They’re systemic failures that put real people at risk. In 2022, the FDA withdrew approval for a breast cancer drug that had been prescribed to over 15,000 women for nearly a decade, even though the final study proving it ineffective had been completed two years earlier. Patients kept taking it because no one told them it no longer met safety standards. This isn’t an anomaly. It’s the old system at work.
How a Drug Gets Approved-And Why That’s Not the End of the Story
When a drug is approved by the FDA, it doesn’t mean it’s perfect. It means the benefits outweigh the known risks, based on the data available at the time. For many new drugs-especially in cancer, rare diseases, and neurology-the FDA uses what’s called accelerated approval. This lets drugs reach patients faster, based on early signs of benefit, like tumor shrinkage or lab results, rather than proof that people live longer or feel better. But here’s the catch: companies have to run follow-up studies to confirm those early results. If they don’t, or if the follow-up proves the drug doesn’t help, the FDA is supposed to pull it. For years, that didn’t happen. Take Makena, a drug approved in 2011 to prevent preterm birth. By 2020, a large study showed it didn’t work. But it stayed on the market for another two years. Why? The process was slow, unclear, and full of delays.The Old System: Years of Waiting While Patients Kept Taking Risky Drugs
Before 2023, the FDA had no real timeline for pulling a drug. Once a study showed a drug failed, the agency could take up to four years to act. In oncology, where time is everything, this delay was deadly. A 2023 study found that 26% of drugs approved under accelerated pathways eventually got pulled. And during the wait, up to 41% of eligible patients with small cell lung cancer were still getting these drugs-even though they offered no benefit. Doctors didn’t always know a drug was under review for withdrawal. Pharmacists struggled to track which drugs were officially pulled from the FDA’s Orange Book. Patients, meanwhile, trusted their prescriptions. One woman in Ohio told her support group: “I was on a drug for 18 months. My oncologist said it was the best option. Then one day, he said, ‘We’re stopping it. The FDA pulled it.’ I felt lied to.”The 2023 Fix: A New Law That Actually Moves Fast
In December 2023, Congress passed the Consolidated Appropriations Act-and with it, a game-changing rule. For the first time, the FDA has a clear, fast-track process to remove drugs that fail to deliver. Under this law, the agency can act if:- The drug company doesn’t do the required follow-up study on time
- The study proves the drug doesn’t work
- Real-world data shows it’s unsafe or ineffective
- The company lied in its marketing
Who Gets Hurt When Drugs Stay Too Long?
It’s not just patients. Doctors, pharmacies, insurers, and hospitals all scramble when a drug vanishes suddenly. Oncology clinics report it takes an average of 72 hours to find a replacement treatment after a withdrawal. That’s three days without a plan for someone with aggressive cancer. Pharmacists are often the last to know. A 2022 survey found 63% had trouble reading the FDA’s withdrawal notices in the Orange Book. Insurance companies kept paying for drugs they didn’t know were pulled. Patients kept filling prescriptions-until their pharmacy said, “We don’t carry this anymore.” And the cost? The FDA estimates that between 2010 and 2020, withdrawn drugs cost the U.S. healthcare system over $8 billion. That’s money spent on treatments that didn’t work.How the U.S. Compares to the Rest of the World
Other countries have been doing this better for years. The European Medicines Agency and Health Canada use “conditional approval,” which means they approve drugs with strict rules: if you don’t prove it works in two years, it’s gone. The FDA didn’t have that power-until now. The 2023 law borrowed ideas from Europe. It’s not perfect, but it’s a major shift. The FDA now has the tools to match global standards. The question isn’t whether the U.S. can keep up-it’s whether it will use the tools it now has.
What’s Next? Real-World Data and Faster Decisions
The FDA is now testing a new system using real-world data from Flatiron Health, which tracks millions of patient records. Instead of waiting for a company to run a slow, expensive trial, regulators can now look at what’s actually happening in clinics. Did patients live longer? Did their symptoms improve? Did they have more side effects? This could cut withdrawal times even further. In 2024, the FDA launched a pilot program using this data to monitor cancer drugs. Early results show it can flag problems 18 months faster than traditional studies. Industry groups warn this could scare off innovation. If companies fear their drug will be pulled too quickly, they might stop trying to treat rare diseases. But patient advocates say the bigger risk is doing nothing. “We’ve waited too long,” says the Cancer Research Institute. “Now the FDA has the power to act. Let’s see them use it.”What You Should Know If You’re Taking a New Drug
If you’re on a drug approved under accelerated approval-especially for cancer, MS, or rare diseases-ask your doctor:- Is this drug approved under accelerated approval?
- When is the follow-up study due?
- Has the FDA issued any notices about this drug?
Why This Matters Beyond Prescription Bottles
Drug withdrawals aren’t just about pills. They’re about trust. When patients learn their doctor prescribed a drug that later got pulled for being useless, they lose faith in the system. That’s harder to fix than any regulation. The 2023 changes show that when regulators listen to patients, scientists, and frontline doctors, they can move fast. The Makena case wasn’t just a failure-it was a warning. And now, the FDA has a chance to prove it learned.What’s the difference between a drug recall and a withdrawal?
A recall means the manufacturer pulls a specific batch of a drug because of contamination, labeling errors, or manufacturing defects. A withdrawal means the FDA removes the entire drug from the market because it’s unsafe or ineffective. Recalls are about quality. Withdrawals are about safety and performance.
Can a drug be withdrawn even if it’s still being sold?
Yes. The FDA considers a drug withdrawn when the company stops distributing it due to safety or effectiveness concerns-even if some bottles are still in pharmacies or homes. Once the FDA declares a withdrawal, the drug can no longer be legally sold or prescribed. Pharmacies are required to stop dispensing it.
How do I know if a drug I’m taking has been withdrawn?
Check the FDA’s monthly Determination of Safety or Effectiveness list in the Federal Register. Your pharmacist should also be notified. If you’re unsure, ask your doctor or call the FDA’s Drug Information line. Don’t rely on pharmacy labels alone-they may not update immediately.
Why do some drugs stay on the market for years after being proven ineffective?
Before 2023, the FDA had no legal deadline to act. Companies could delay submitting studies, argue over data, or appeal decisions. The process was opaque, and regulators lacked authority to force quick action. The Makena case took over four years to withdraw, even after the study proving it useless was published.
Are generic versions of withdrawn drugs still available?
No. Once a brand-name drug is withdrawn for safety or effectiveness reasons, generic versions can no longer be approved or sold. The FDA removes the drug from the Orange Book, which is the official list of approved drugs that generics can copy. Any existing generic stock must be recalled.
Is it safe to take a drug that’s under review for withdrawal?
If the FDA hasn’t officially withdrawn the drug yet, it’s still legally available. But if you’re on a drug with pending withdrawal-especially one approved under accelerated approval-talk to your doctor. There may be safer, proven alternatives. Don’t wait for a notice. Ask now.

Suresh Patil
November 1, 2025 AT 05:15It’s wild how long it took for the FDA to get a real timeline. In India, we don’t have the same infrastructure, but even our drug regulators act faster when evidence piles up. I remember when a diabetes med got pulled here after three patients had heart issues-no 4-year waiting game. Just a notice, then gone. Maybe the U.S. is finally catching up to how the world actually works.
Ram Babu S
November 1, 2025 AT 11:31My uncle was on one of those accelerated drugs for pancreatic cancer. Took it for 14 months. Then one day, his oncologist said, 'We’re switching.' No warning. No explanation. Just... 'it’s not working anymore.' He felt like a lab rat. I hope this new law means fewer people get blindsided like that.
Kyle Buck
November 2, 2025 AT 00:09The structural inefficiencies in the FDA’s prior regulatory framework were profoundly concerning, particularly given the accelerated approval pathway’s inherent reliance on surrogate endpoints. The absence of enforceable timelines for post-marketing commitments created a pernicious moral hazard, wherein pharmaceutical entities could defer confirmatory trials indefinitely, thereby prolonging patient exposure to therapeutically inert agents. The 2023 legislative intervention represents a necessary recalibration toward evidence-based governance, though the continued reliance on industry-submitted data remains a latent vulnerability.
Amy Craine
November 2, 2025 AT 08:07I work in oncology pharmacy, and let me tell you-the chaos when a drug gets pulled is unreal. We had to scramble to find alternatives for six patients in one day last year. No one had been told the drug was under review. The FDA’s old system was a disaster for frontline staff. This new 180-day rule? It’s not perfect, but at least now we can plan. Patients deserve transparency, not last-minute surprises.
Alicia Buchter
November 3, 2025 AT 21:44Ugh. I can’t believe we’re still talking about this. Like, wow, the FDA finally got around to doing something basic? Meanwhile, Europe’s been doing this since 2010. And now we’re patting ourselves on the back like it’s a miracle? Please. The real scandal is that it took this long. I’m just glad my insurance stopped paying for that nonsense before I got stuck on it.
M. Kyle Moseby
November 4, 2025 AT 21:32This is why you can’t trust the government. They let dangerous drugs stay on shelves for years. Then they act like heroes when they finally do something right. I don’t need a law to tell me not to take junk medicine. People just need to stop being lazy and do their own research.
Zach Harrison
November 6, 2025 AT 10:43the 2023 fix is a big deal but honestly? it’s still too slow. i had a friend on an ALS drug that got pulled after 8 months of waiting even under the new rules. real-world data is the way to go-why wait for a company to finish a trial when we’ve got millions of records showing it’s useless? also, why is the orange book still so hard to read? someone needs to make a simple app for this.
Terri-Anne Whitehouse
November 6, 2025 AT 17:20Let’s be honest-this entire system is a performative gesture. The FDA didn’t act out of moral clarity; they were pressured by patient advocacy groups and media scrutiny. The real issue isn’t the timeline-it’s that the entire accelerated approval model is a corporate loophole disguised as medical progress. The fact that we’re celebrating a 180-day window as progress is depressing. In the UK, we’d have pulled it within 60 days. And yes, I’ve read the literature. You haven’t.
Matthew Williams
November 8, 2025 AT 14:58So now the FDA gets to be the drug police? Who the hell gave them that power? You think Big Pharma’s gonna stop making drugs because of this? Nah. They’ll just move to China or India where regulations don’t exist. Meanwhile, Americans are gonna die because we’re too busy punishing companies instead of letting them innovate. This isn’t safety-it’s socialism with a white coat.