Drug Interaction Issues: When Generics Interact Unexpectedly
 Dec, 20 2025
Dec, 20 2025
People assume generic drugs are just cheaper copies of brand-name meds. That’s mostly true - same active ingredient, same dose, same effect. But when someone switches from a brand-name drug to a generic and suddenly feels off, it’s easy to blame the generic. Drug interaction issues don’t suddenly appear because a pill is cheaper. They’re caused by the chemistry inside the pill, not the label. So why do people think generics behave differently?
Generics Are Supposed to Work the Same
The U.S. Food and Drug Administration requires generic drugs to prove they’re bioequivalent to the brand-name version. That means the body absorbs the active ingredient at nearly the same rate and amount - within 80% to 125% of the original. For most drugs, that tiny variation doesn’t matter. A blood pressure pill that’s 90% absorbed instead of 100%? Still works fine. But for drugs with a narrow therapeutic index - like warfarin, levothyroxine, or phenytoin - even small changes can tip the balance. That’s why the FDA demands tighter standards for these: 90% to 112% bioequivalence. It’s not about brand or generic. It’s about the drug’s chemistry.
What Actually Causes the Problems?
The real culprits aren’t the active ingredients. They’re the extras. Inactive ingredients - things like lactose, dyes, preservatives, or fillers - don’t treat your condition. But they can trigger reactions in sensitive people. One patient in 2021 had stomach cramps and bloating after switching to a generic version of levothyroxine. The brand version used corn starch. The generic used lactose. The patient was lactose intolerant. No change in thyroid hormone. Just a bad reaction to a filler.
Another example: some generic sertraline uses sodium benzoate as a stabilizer. The brand version uses hydrochloride salt. For most people, no difference. But if someone is on a low-sodium diet or has kidney issues, that extra sodium might add up. It’s not a drug interaction. It’s a food-medication interaction hiding in plain sight.
Why Do People Think Generics Cause More Side Effects?
Psychology plays a big role. If you’ve been told generics are “inferior,” or you’ve heard stories about people getting sick after switching, your brain starts looking for proof. That’s called the nocebo effect - the opposite of placebo. You expect to feel worse, so you do. A 2022 Kaiser Family Foundation survey found 47% of patients believed generics worked differently. But when researchers checked medical records, only 3.7% of those reports matched actual physiological changes.
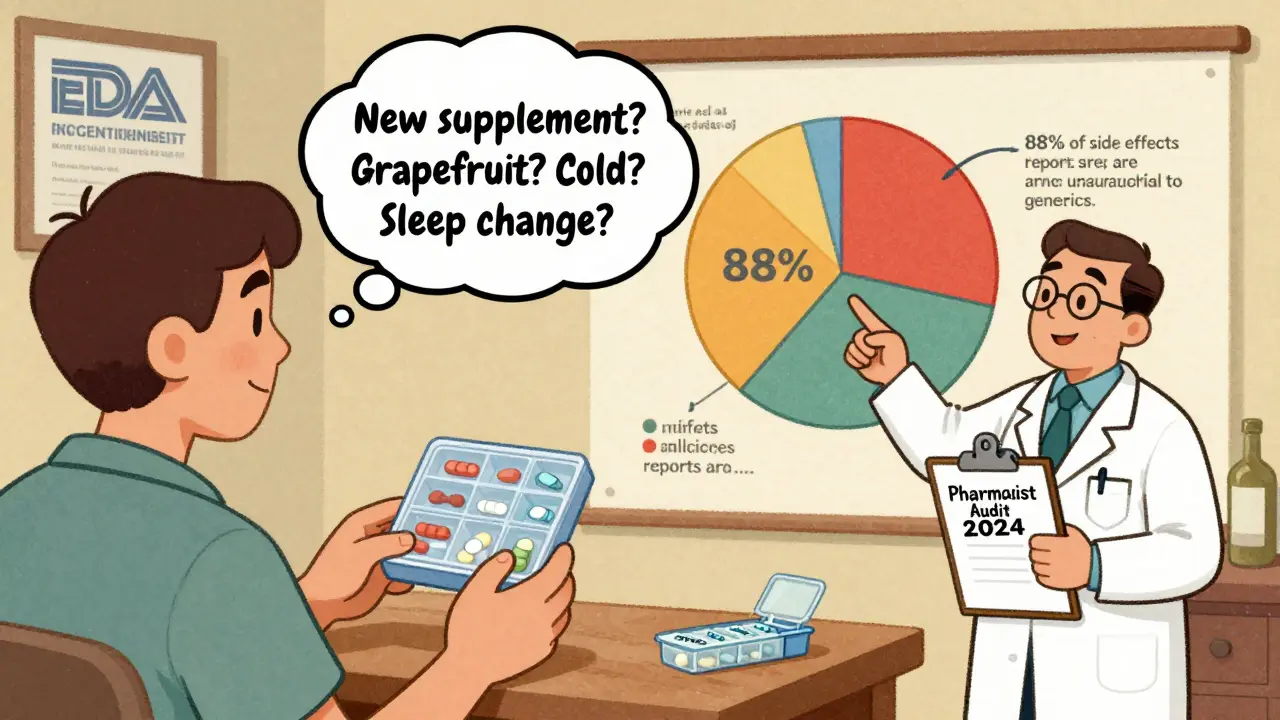
On Reddit’s r/pharmacy, 62% of respondents said patients complained about generics causing new side effects. But pharmacists who actually track outcomes said only 18% of those complaints had any real basis. The rest? Timing. Maybe the patient started a new supplement. Or ate more grapefruit. Or skipped a dose. Or got a cold. But the switch to generic became the scapegoat.

Drug Interactions Don’t Care About Brand Names
Here’s the hard truth: drug interactions happen because of what’s in the pill, not who made it. Fluconazole - whether brand or generic - can spike simvastatin levels by 300-400%. Grapefruit juice - whether you’re on brand or generic - blocks the enzyme that breaks down calcium channel blockers. That’s not a generic problem. That’s a pharmacology problem.
The FDA requires generic manufacturers to include the exact same interaction warnings as the brand-name drug. In 2022, their audit showed 100% compliance. If your brand-name pill says “avoid grapefruit,” your generic does too. The label doesn’t change. The risk doesn’t change. Only the price does.
When Switching Generics Gets Risky
Here’s where things get messy. You might take the same generic drug for months. Then your pharmacy switches to a different manufacturer. Same name. Same dose. But different fillers. Different shape. Different color. And suddenly, you feel weird.
In 2022, IQVIA found that 32% of U.S. prescriptions switched between generic manufacturers at least once. For most people, no problem. But for those on warfarin, thyroid meds, or seizure drugs, it’s a red flag. The American Society of Health-System Pharmacists recommends hospitals stick to one generic manufacturer for these drugs. Why? Consistency. Not because one is better. But because switching increases the chance of a hidden reaction - even if it’s just psychological.
The FDA’s MedWatch system recorded 1,842 adverse event reports linked to generic switches in 2022. Only 11.8% involved actual interaction issues. The rest? Adherence problems. Confusion. Misunderstanding. That’s why pharmacists are now trained to ask: “Did you switch generics recently?” - not just “Are you taking your meds?”
What You Can Do
- Stick with the same generic manufacturer if you’re on a narrow therapeutic index drug. If your pharmacy switches, ask if you can keep your current version.
- Check the inactive ingredients. Look at the package insert or ask your pharmacist. If you’re allergic to lactose, gluten, or dyes, know what’s in your pill.
- Don’t assume a new side effect means the drug is broken. Track changes: Did you start a new supplement? Change your diet? Get sick? Adjust your sleep? Those matter more than the pill’s brand.
- Use a pill organizer. Missing doses or taking extra pills is a bigger risk than switching generics.
- Ask your pharmacist to review all your meds - including OTC and supplements - every time you refill. Interactions don’t care if it’s brand or generic. They care if you’re mixing them.
The Bigger Picture
Generics make up 90% of prescriptions in the U.S. They save billions. But misconceptions cost money too. A 2023 Health Affairs study found that 1.2 million unnecessary brand-name prescriptions are filled every year because people fear generics cause problems. That adds up to $8.7 billion in extra costs.
The FDA launched a $15 million campaign in January 2024 to fix this. It’s not about convincing people generics are safe. It’s about teaching them how to think about drug interactions - the real ones, not the imagined ones.
Bottom line: A generic drug doesn’t become dangerous just because it’s cheaper. The active ingredient is the same. The interaction risks are the same. The warnings are the same. The only thing that changes is who made it - and whether you know what’s in the filler.

Siobhan K.
December 20, 2025 AT 20:59Let me guess - someone switched generics and blamed the pill when they started eating more grapefruit and sleeping 4 hours a night. The real issue? People don’t track their own habits, then pin it on a $0.50 pill.
Brian Furnell
December 21, 2025 AT 03:30From a pharmacokinetic standpoint, the bioequivalence threshold (80–125%) is statistically robust for most therapeutics - but for drugs with a narrow therapeutic index (NTI), such as warfarin or levothyroxine, even marginal deviations in Cmax or AUC can precipitate subtherapeutic or toxic outcomes. The FDA’s 90–112% NTI-specific criterion is prudent, yet real-world variability in excipient profiles introduces confounding variables that aren't captured in bioequivalence studies.
Jason Silva
December 21, 2025 AT 10:18THEY KNOW. THEY KNOW THE BRAND NAMES MAKE MORE MONEY. THE FDA IS IN BED WITH BIG PHARMA. WHY DO YOU THINK THEY LET THEM CHANGE THE COLOR AND SHAPE? IT’S A TRICK TO MAKE YOU THINK IT’S DIFFERENT SO YOU’LL BUY THE EXPENSIVE ONE AGAIN 😈💊
mukesh matav
December 22, 2025 AT 14:52My aunt took generic levothyroxine and felt fine. Then she switched to another generic and got dizzy. Turned out the new one had a different dye. She’s fine now that she’s back on the original generic. Just ask your pharmacist - it’s not that hard.
Peggy Adams
December 24, 2025 AT 06:01So you’re telling me I paid $200 for a brand-name pill and now I’m supposed to believe this $4 generic is exactly the same? I don’t buy it. My head feels weird. Coincidence? I think not.
Sarah Williams
December 24, 2025 AT 06:16Great breakdown. Seriously, if you’re on a narrow therapeutic index drug, stick with one manufacturer. And check those fillers. It’s not rocket science - just common sense.
Theo Newbold
December 26, 2025 AT 01:31The 1.2 million unnecessary brand-name prescriptions? That’s not misinformation - that’s corporate greed disguised as patient care. The FDA’s $15M campaign is a PR stunt. They don’t want you to know how much they’ve been complicit in letting generics vary in excipients while claiming bioequivalence.
Jackie Be
December 27, 2025 AT 01:16OMG I switched to generic sertraline and suddenly I was crying at my cat’s sneeze 😭 turns out it had sodium benzoate and I’m on a low sodium diet… my pharmacist didn’t tell me anything!!
John Hay
December 28, 2025 AT 09:42I’ve been taking the same generic for 5 years. Then they changed the pill and I felt like crap. Called my doc. He said, ‘Check the label.’ Found out it had lactose. I’m lactose intolerant. Never switched back. Simple fix. Pharmacist should tell you this stuff. They don’t. That’s the real problem.