Doctor Attitudes Toward Generic Drugs: What Providers Really Think
 Feb, 10 2026
Feb, 10 2026
For decades, generic drugs have been the quiet workhorse of modern healthcare - cheaper, just as effective, and approved by the same agencies that regulate brand-name pills. Yet many doctors still hesitate to prescribe them. Why? It’s not about cost alone. It’s about trust, experience, and what doctors think they know.
What Doctors Believe About Generic Drugs
A 2017 study of 134 physicians in Greece found that more than a quarter of them believed generic medications were less effective than brand-name versions. That number isn’t outdated. Even today, surveys show that around 27% of doctors still question whether generics deliver the same therapeutic results. This isn’t just about ignorance. It’s rooted in real clinical experiences.
Some doctors report cases where patients had unexpected side effects after switching from a brand-name drug to a generic. A common example? Levothyroxine. Patients on this thyroid medication often notice subtle changes in energy, weight, or heart rate after a generic switch. While clinical trials prove bioequivalence - meaning the body absorbs the drug within 80-125% of the brand - real patients don’t live in controlled trials. They live with daily symptoms. When a patient says, “This generic doesn’t feel the same,” a doctor listens.
Even more telling: a 2023 study in the Journal of Young Pharmacists found that 83.4% of medical practitioners believe doctors need more education on generics. That’s not a small group. That’s nearly every doctor in the room. And it points to a deeper problem: many physicians were never properly trained on how generics actually work.
Who Thinks Differently? Demographics Matter
Not all doctors view generics the same way. The data shows clear patterns. Male physicians, specialists, and those with over 10 years of experience are significantly more skeptical than their female peers or younger colleagues. In fact, the Greek study found statistically significant differences - p-values under 0.05 - confirming that experience doesn’t always mean openness. In some cases, it means rigidity.
Age plays a role too. The PLOS ONE 2018 study showed a strong correlation between age and negative attitudes. Older doctors were less likely to believe generics were equally effective, less likely to accept substitution, and less likely to see the cost-benefit. It’s not that they’re resistant to change - it’s that their training happened before modern bioequivalence standards were widely understood.
And then there’s the pharmacist contrast. Pharmacists, who handle generics daily, are far more confident. Only 22.1% of pharmacists doubted therapeutic equivalence, compared to 28.7% of physicians. That gap isn’t accidental. Pharmacists see the manufacturing process. They know that a generic made in India is held to the same standards as one made in Ohio. Doctors rarely do.
The Knowledge Gap Is Real
Here’s a startling stat: only 43.7% of primary care physicians correctly understood the FDA’s bioequivalence range - even though 78.4% claimed they were familiar with the regulations. That’s a massive disconnect. You can’t trust what you don’t understand.
Many doctors think generics must be stronger to work - so they assume they cause more side effects. Some believe different manufacturers produce inconsistent quality. And while the FDA requires all generics to meet strict standards, the reality is more complex. A pill from one company might have slightly different fillers or coatings, which can affect absorption in sensitive patients. That’s not a flaw in regulation - it’s a biological nuance. But without proper education, doctors interpret it as a failure of the generic system.
The same study that found low bioequivalence knowledge also showed that 74.3% of physicians felt they didn’t have enough time during patient visits to explain generics. And 86.1% said they hadn’t received any continuing education on generics in the past five years. That’s not negligence. It’s a system failure.
Why This Matters Beyond Prescriptions
Doctors don’t just write prescriptions. They shape beliefs. A 2012 CDC study found that 68.4% of patients learn about generic drugs from their doctors. If a doctor says, “I’d stick with the brand,” the patient believes it. If a doctor says, “This generic is just as good,” the patient is far more likely to take it.
But when doctors are unsure, they say nothing. And silence speaks louder than advice. In rural clinics, 41.7% of patients stopped taking their medication because they didn’t trust the generic - not because it didn’t work, but because their doctor didn’t explain it well. That’s not a drug failure. It’s a communication failure.
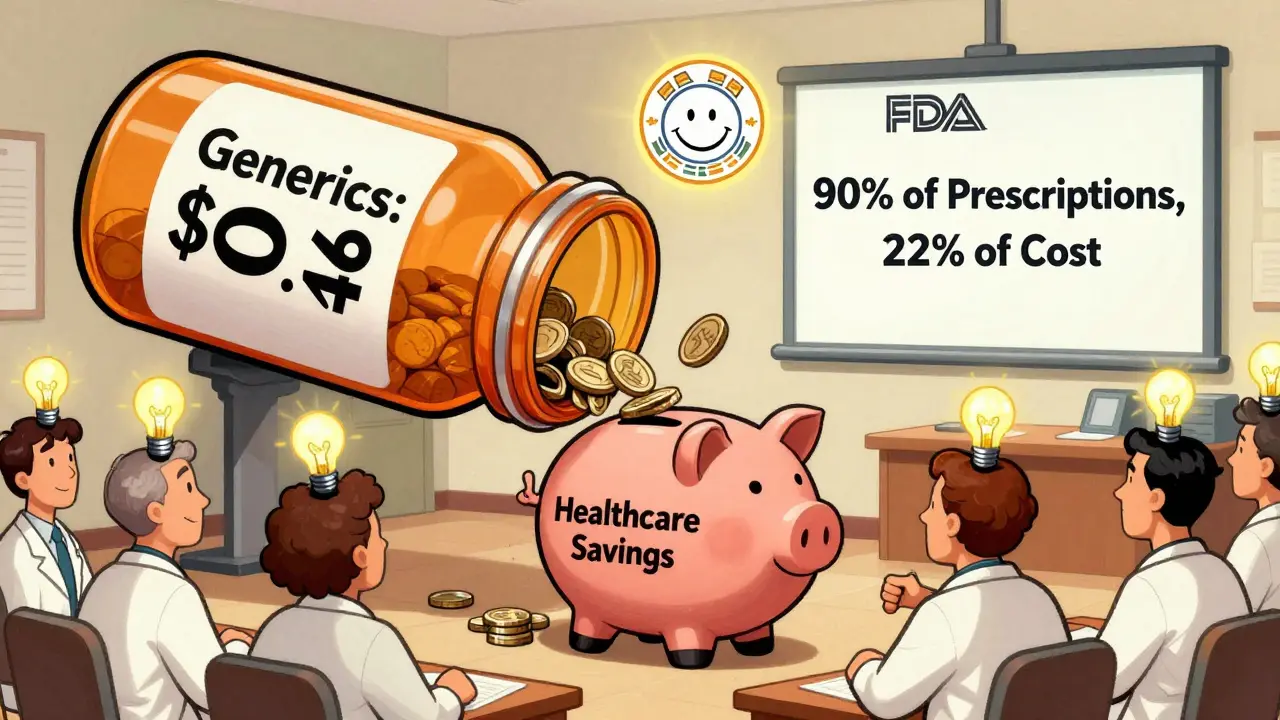
And the cost? The U.S. spends $528 billion annually on generic drugs. They make up 90% of prescriptions but only 22% of spending. That’s $400 billion in savings every year - money that could go to mental health, diabetes care, or preventive services. But if doctors don’t prescribe them, those savings vanish.
What’s Changing? Education Is Working
There’s good news. When doctors get clear, evidence-based information, their attitudes shift.
The Greek study gave a group of physicians a 90-minute workshop on bioequivalence, manufacturing standards, and real-world outcomes. Six months later, their generic prescribing rates jumped by 22.5%. The biggest boost? Doctors with 5-10 years of experience - not the veterans, not the rookies. The ones still forming their habits.
Peer educators made a huge difference. Doctors who had successfully switched to high generic prescribing were 43.2% more influential than outside trainers. Why? Because they’d been there. They’d worried about levothyroxine too. They’d seen patients struggle. And then they’d tried it - and it worked.
At Johns Hopkins, when providers were given real-world data on newly approved generics - not just lab numbers, but actual patient outcomes - prescribing rates rose by 28.6%. That’s not magic. That’s transparency.
The Way Forward
Fixing this isn’t about pushing generics. It’s about rebuilding trust. That means:
- Medical schools need to teach bioequivalence early and often - right now, only 38.7% of U.S. med schools do.
- Continuing education should be mandatory, not optional. Quarterly updates on new generics, side effect patterns, and manufacturing changes could rebuild confidence.
- Communication tools for doctors - simple handouts, scripts, or digital prompts - can help explain generics to patients without wasting time.
- Standardized naming is coming. The AMA’s 2024 push for pronounceable generic names (instead of long chemical labels) will help doctors feel more comfortable saying them aloud.
The biggest barrier isn’t science. It’s perception. And perception can change - if we give doctors the facts, the tools, and the space to rethink what they thought they knew.
Generics aren’t second-rate. They’re science-tested, cost-effective, and used by millions every day. But until doctors believe it - truly believe it - patients will keep paying more than they have to.
