Cervical Myelopathy: Recognizing Spinal Stenosis Symptoms and When Surgery Is Needed
 Dec, 3 2025
Dec, 3 2025
When your hands start fumbling with buttons, your walk feels unsteady, or you suddenly drop things you’ve held for years, it’s easy to blame aging. But if these changes are new, worsening, and happening without injury, they could signal something more serious: cervical myelopathy. This isn’t just a stiff neck. It’s your spinal cord being squeezed in your neck, and if ignored, it can lead to permanent nerve damage.
What Exactly Is Cervical Myelopathy?
Cervical myelopathy happens when the spinal cord in your neck gets compressed. The most common cause? Cervical spinal stenosis - a narrowing of the bony canal that protects your spinal cord. Think of it like a water pipe that’s slowly getting clogged. Over time, bone spurs grow, discs flatten, ligaments thicken, and the space for your spinal cord shrinks. When it drops below 13 millimeters, it’s considered stenosis. At 10 mm or less, you’re in the danger zone. This isn’t rare. About 9% of people over 70 have it. And it’s the leading cause of spinal cord problems in adults over 55. The most common type, called cervical spondylotic myelopathy (CSM), makes up 75% of cases. It doesn’t come on overnight. It creeps in slowly, which is why many people wait years before seeking help.Early Signs You Can’t Ignore
The symptoms of cervical myelopathy are subtle at first but get harder to brush off. You might notice:- Your fingers feel clumsy - you drop keys, struggle with zippers, or can’t button a shirt like you used to.
- Your walk changes. You feel unsteady, like you’re walking on a boat, or you bump into things more often.
- You have trouble balancing, especially in the dark or on uneven ground.
- Your arms or hands go numb or tingle, often worse at night.
- You feel stiffness or pain in your neck, but surprisingly, about half of people with myelopathy don’t have neck pain at all.
- You start having trouble controlling your bladder - feeling sudden urgency or even leaking.
How Doctors Diagnose It
A simple X-ray won’t cut it. You need an MRI - the gold standard. It shows not just the narrowing of the canal, but also whether the spinal cord itself is injured. Look for bright spots on T2-weighted images - that’s swelling or scarring inside the cord, a clear sign of myelopathy, not just stenosis. Doctors also use the Japanese Orthopaedic Association (JOA) score. It’s a quick test that checks your arm strength, leg function, sensation, and bladder control. A score below 14 means you have myelopathy. A score under 12? That’s moderate to severe, and surgery is usually recommended. EMG and nerve tests can catch early nerve damage before you even feel it. But MRI is the deciding factor. About 21% of people over 40 have stenosis on MRI but no symptoms. That’s why diagnosis isn’t just about the scan - it’s about matching the scan to your symptoms.Can You Avoid Surgery?
If your symptoms are mild and stable - say, just a little clumsiness with no balance issues - your doctor might suggest watchful waiting. Physical therapy, NSAIDs, and avoiding activities that strain your neck can help manage symptoms. But don’t be fooled: only 28% of people with mild myelopathy improve with conservative care over two years. Nearly two-thirds get worse. There’s no magic pill to reverse spinal cord damage. Once nerve fibers are crushed, they don’t regenerate. That’s why timing matters more than anything.When Surgery Becomes Necessary
If your JOA score is below 12, or if you’re getting worse - even slowly - surgery is the only proven way to stop progression and improve function. Studies show 70% to 85% of patients get better after surgery. The key is doing it before the cord is permanently damaged. There are two main surgical approaches:- Anterior (front): ACDF (anterior cervical discectomy and fusion) or disc replacement. Best for one or two levels. Success rate: 85-90%. You’ll likely go home in 1-2 days.
- Posterior (back): Laminectomy, laminoplasty, or fusion. Better for three or more levels or if your neck is curved the wrong way. Laminoplasty opens the back of the spine like a door - preserves motion, less neck pain afterward, but slightly slower recovery.
What Happens After Surgery?
Recovery takes time. Most people are back to light activities in 4-6 weeks. Full recovery - including regaining strength and balance - can take 3 to 6 months. You’ll need physical therapy. About 85% of patients do 8-12 weeks of rehab focused on gait training and neck stability. You might have temporary side effects: trouble swallowing (common after front surgery), neck stiffness, or mild pain. About 22% of people have swallowing issues for the first few months. Around 18% of those who have posterior surgery develop chronic neck pain later - known as post-laminectomy syndrome. But the biggest win? Hand function. Eighty-two percent of patients report better grip and dexterity within a year. Gait improvement is less guaranteed - only 65% regain normal walking, and 28% still need a cane or walker.Why Timing Is Everything
Delaying surgery is the biggest mistake people make. Every month you wait, you lose about 3% of your recovery potential. A 2023 study found patients who had surgery within six months of symptoms started improved 37% more than those who waited over a year. One patient, a 68-year-old retired teacher, waited 18 months after noticing her fingers wouldn’t hold pens. By the time she had surgery, she could barely tie her shoes. She got better - but never regained her handwriting. Another patient, diagnosed within two months of hand clumsiness, was back to knitting and gardening in four months.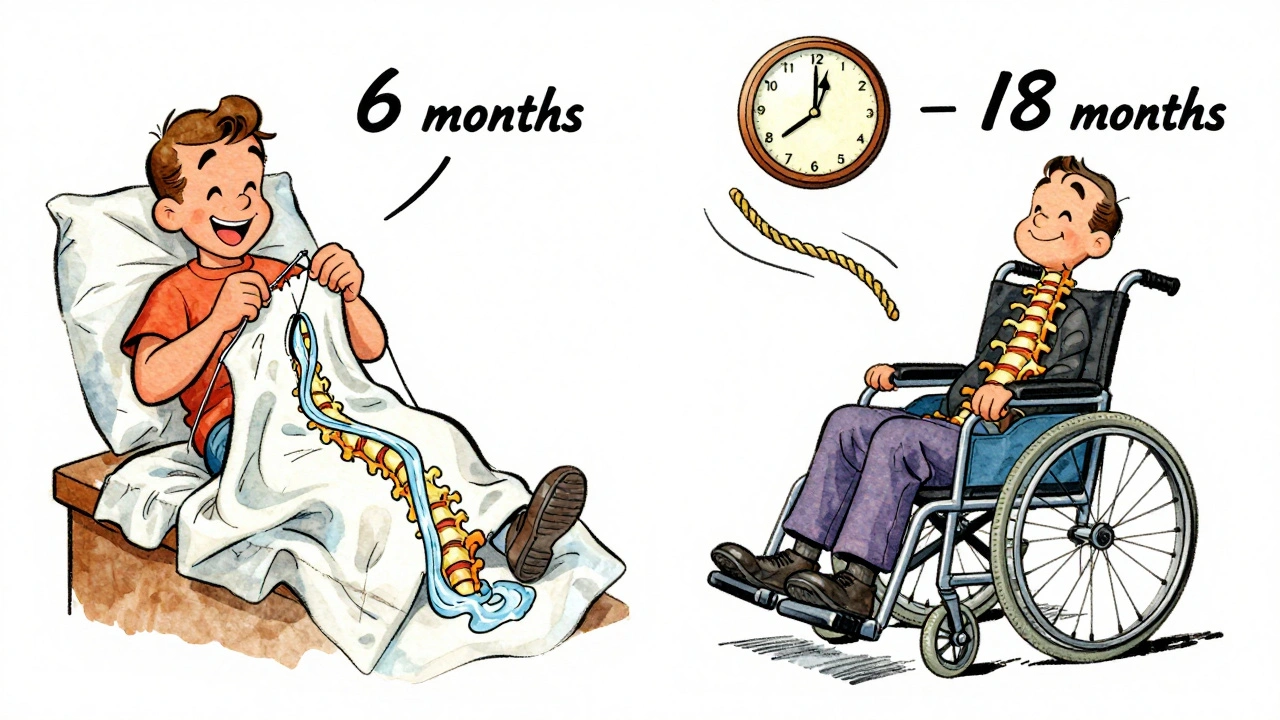
What You Can Do Right Now
If you’re experiencing any of these symptoms:- See your doctor. Don’t wait for it to get worse.
- Ask for an MRI of your cervical spine - not just X-rays.
- Get a referral to a spine specialist, not just a general neurologist.
- If you smoke, quit. Smoking cuts fusion success rates by half.
- If you’re diabetic, get your HbA1c under 7.0. High blood sugar raises infection risk.
- Start gentle neck and core strengthening. Don’t wait for surgery to build support.
What’s New in Treatment
The field is moving fast. In 2023, the FDA approved the M6-C artificial disc for two- and three-level surgeries - a big step forward. Unlike fusion, it keeps your neck moving. Early results show 81% of patients kept motion at two years. Minimally invasive techniques are cutting hospital stays and blood loss. Robotic-assisted surgery is coming - expected to reduce revision rates by nearly a third by 2030. But experts warn: surgery rates have jumped 33% since 2010, and 15-20% of those operations may be unnecessary. The goal now isn’t just to operate - it’s to operate on the right person, at the right time.Final Thoughts
Cervical myelopathy isn’t something you can out-wait. It doesn’t heal on its own. The longer you wait, the less you’ll recover - even with surgery. Early symptoms like clumsy hands or unsteady walking aren’t just part of getting older. They’re red flags. If you’ve noticed these changes, don’t brush them off. Get an MRI. See a specialist. The window to protect your nerves is narrow - but it’s open.Can cervical myelopathy get better without surgery?
In rare cases, mild symptoms may stabilize with rest and physical therapy, but true improvement without surgery is uncommon. Studies show only about 28% of patients with mild myelopathy get better over two years without surgery, while 63% get worse. Once nerve damage occurs, it doesn’t reverse on its own.
How do I know if my symptoms are from myelopathy and not something else?
Myelopathy has a specific pattern: hand clumsiness, gait imbalance, and increased reflexes in the knees and ankles. If you have numbness in your hands AND trouble walking, it’s likely spinal cord-related. Other conditions like carpal tunnel or Parkinson’s affect different nerves or show different signs. An MRI and neurological exam are needed to confirm.
Is cervical myelopathy the same as spinal stenosis?
No. Spinal stenosis is the narrowing of the spinal canal. Myelopathy is the damage to the spinal cord caused by that narrowing. You can have stenosis without myelopathy - many people do. But if you have myelopathy, you have stenosis too. The key difference is neurological symptoms.
What’s the success rate of cervical myelopathy surgery?
About 70-85% of patients see significant improvement in strength, coordination, and bladder control after surgery. Success depends on how advanced the damage was before surgery. Patients treated within six months of symptoms have the best outcomes - up to 2.7 times more likely to report excellent recovery.
How long does recovery take after cervical myelopathy surgery?
Most people return to light activities in 4-6 weeks. Full recovery - including regaining balance and fine motor skills - takes 3 to 6 months. Physical therapy is critical. About 85% of patients need 8-12 weeks of rehab focused on walking and hand function. Some may need ongoing support for balance or weakness.
Are there risks with cervical spine surgery?
Yes. Major complications occur in 4-6% of cases, including difficulty swallowing, C5 nerve palsy (weak shoulder), or, rarely, worsening neurological symptoms. The risk is higher with posterior surgery or if you’re older or have other health issues. But the risk of not treating progressive myelopathy - permanent paralysis or loss of function - is far greater.

Abhi Yadav
December 3, 2025 AT 19:33Julia Jakob
December 4, 2025 AT 17:12Robert Altmannshofer
December 5, 2025 AT 23:26Kathleen Koopman
December 6, 2025 AT 01:45Nancy M
December 6, 2025 AT 06:52gladys morante
December 7, 2025 AT 08:21David Ross
December 7, 2025 AT 22:14Craig Ballantyne
December 8, 2025 AT 12:53Victor T. Johnson
December 10, 2025 AT 02:43Nicholas Swiontek
December 10, 2025 AT 13:17Robert Asel
December 11, 2025 AT 18:37Shannon Wright
December 11, 2025 AT 20:15vanessa parapar
December 12, 2025 AT 19:25Ben Wood
December 13, 2025 AT 06:08Rachel Nimmons
December 14, 2025 AT 13:59Robert Altmannshofer
December 15, 2025 AT 23:33