Antifungals: Liver Safety and Drug Interaction Risks You Can't Ignore
 Dec, 29 2025
Dec, 29 2025
When you take an antifungal pill for a stubborn nail infection or a systemic yeast problem, you’re not just fighting fungus-you’re putting your liver on the line. Many people assume these drugs are safe because they’re common, over-the-counter, or prescribed by a doctor. But the truth is, some antifungals carry serious risks that can quietly damage your liver-sometimes without warning.
Not All Antifungals Are Created Equal
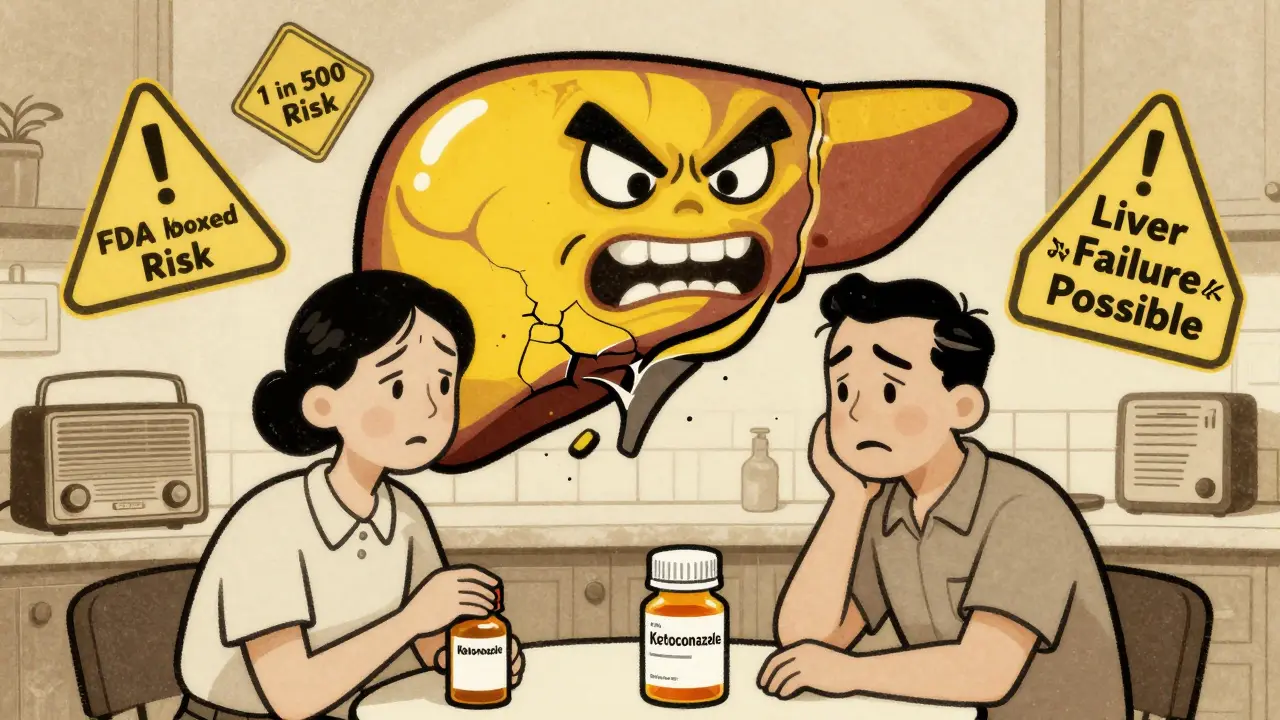
There are four main classes of antifungal drugs: azoles, polyenes, echinocandins, and allylamines. Each works differently, and each carries a different level of liver risk. The most widely used are the azoles-fluconazole, itraconazole, voriconazole, and ketoconazole. But here’s the catch: not all azoles are equal when it comes to liver safety.Ketoconazole, once a go-to for fungal infections, is now one of the most dangerous. The FDA issued a boxed warning in 2013 after reports showed it caused severe liver injury in about 1 in 500 users. Some cases led to liver failure and transplant. Because of this, it’s no longer used for common infections like athlete’s foot or ringworm. In Europe, it was pulled from the market entirely in 2013. Even in the U.S., it’s restricted to rare, life-threatening fungal infections when nothing else works.
Voriconazole and itraconazole aren’t much safer. Studies show they trigger drug-induced liver injury (DILI) more often than fluconazole. In one analysis of over 17 years of FDA reports, voriconazole had the highest signal for liver damage among azoles. Patients on these drugs often develop elevated liver enzymes within 2 to 8 weeks-sometimes before they even feel sick.
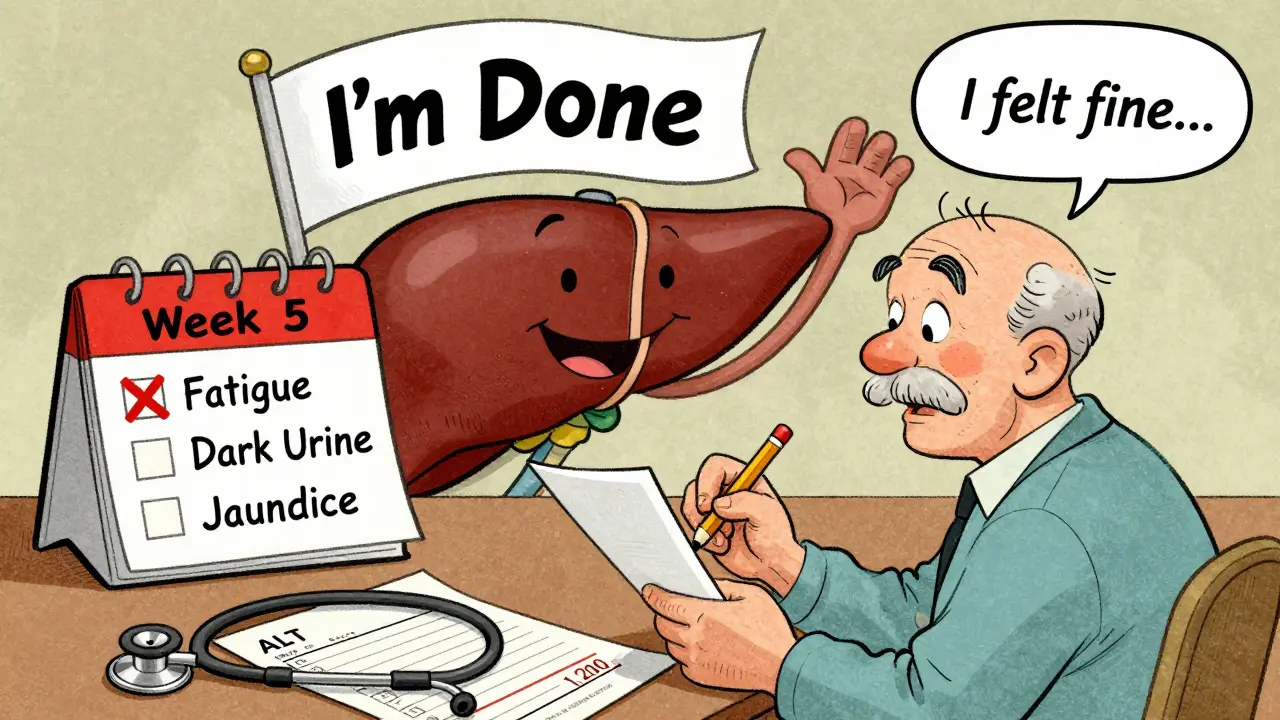
Terbinafine, an allylamine used mostly for nail fungus, has a lower overall risk-about 0.1% of users. But here’s what most people don’t know: it still carries a black box warning for potential liver failure. A patient might feel fine for weeks, then suddenly develop jaundice or extreme fatigue. One case reported on Healthline described jaundice at week five, with symptoms resolving only after stopping the drug.
Echinocandins like caspofungin and micafungin are often seen as safer because they’re given intravenously in hospitals. But don’t be fooled. A 2022 real-world study found echinocandins were linked to DILI more than previously thought. Anidulafungin, in particular, showed the highest death rate among antifungal-related liver injuries-50% in reported cases. That sounds alarming, but it’s likely because these drugs are used in critically ill patients who already have liver problems. So it’s not necessarily the drug itself-it’s the patient’s condition.
Who’s at the Highest Risk?
You might think only people with existing liver disease need to worry. But that’s not true. While pre-existing liver conditions increase risk, many cases happen in otherwise healthy adults.Older adults-especially those over 65-are at much higher risk. Data from Taiwan’s national health database shows the rate of antifungal-induced liver injury jumps from 2.4 cases per 10,000 people per year in the general population to 17.8 cases per 10,000 in seniors. And they’re more likely to die from it.
People taking multiple medications are also at risk. Azoles like voriconazole and itraconazole are metabolized by the liver using the CYP450 enzyme system. That means they interact with dozens of common drugs: statins, blood thinners, antidepressants, even some heart medications. These interactions can cause drug levels to spike, increasing liver toxicity.
One study found that people with a specific genetic variation in the CYP2C19 gene had a 3.7 times higher risk of liver damage from voriconazole. That’s why some hospitals now test for this before prescribing it. Genetic testing isn’t routine yet-but it should be, especially for long-term use.
Alcohol use makes things worse. The FDA specifically warns against mixing ketoconazole with alcohol. Even moderate drinking can push an already stressed liver over the edge.
What Symptoms Should You Watch For?
Liver damage from antifungals doesn’t always show up on blood tests before you feel something. That’s why knowing the early signs is critical.Common early symptoms include:
- Unexplained fatigue
- Nausea or vomiting
- Loss of appetite
- Dark urine
- Yellowing of the skin or eyes (jaundice)
- Pain or discomfort in the upper right side of your abdomen
One Reddit user shared a terrifying story: after three weeks on ketoconazole for a fungal lung infection, their ALT (a liver enzyme) spiked to 1,200 U/L. Normal is 7-56. They ended up in the hospital. Another patient on itraconazole for nail fungus saw their bilirubin climb to 12.3 mg/dL-normal is under 1.2. They spent three weeks in the hospital.
The problem? These symptoms look like the flu, stress, or aging. Many doctors miss the connection. Patients often think, “It’s just a side effect,” and keep taking the drug until it’s too late.

Monitoring Is Not Optional
If you’re prescribed a systemic antifungal, liver monitoring isn’t a suggestion-it’s a requirement.The Infectious Diseases Society of America recommends:
- Baseline liver function tests (LFTs) before starting any systemic antifungal
- Weekly LFTs for the first month for high-risk drugs like ketoconazole, itraconazole, and voriconazole
- Biweekly monitoring for the rest of treatment
- For terbinafine: test at 4-6 weeks, then every 4-6 weeks if treatment lasts longer than 8 weeks
Doctors should stop the drug if:
- ALT or AST levels are more than 3 times the upper limit of normal AND you have symptoms
- ALT or AST levels are more than 5 times the upper limit of normal-even if you feel fine
But here’s the scary part: a 2020 study found only 37.2% of primary care doctors followed these guidelines when prescribing terbinafine for nail fungus. That means over 60% of patients are being put at risk without proper monitoring.
If you’re taking an antifungal and your doctor hasn’t ordered blood work, ask for it. Don’t wait for symptoms. By the time you feel sick, the damage may already be done.
What’s Changing in 2025?
The landscape is shifting fast. Ketoconazole use has dropped by over 90% since the 2013 FDA warning. Hospitals now prefer echinocandins for invasive candidiasis-68% of first-line treatments in 2020, up from just 20% a decade ago.But the real game-changer is precision medicine. In October 2022, researchers identified a genetic marker that predicts voriconazole liver toxicity. Testing for CYP2C19 variants is now being piloted in major cancer centers. In the next few years, this could become standard before prescribing any azole.
The FDA’s Sentinel Initiative, launched in 2008, now uses real-time data from millions of electronic health records to spot liver injury signals before they become widespread. A pilot AI program scheduled for early 2024 will scan adverse event reports automatically to flag risky drug combinations.
New antifungals like olorofim and ibrexafungerp are in development with liver safety built into their design. Early trials show 78% fewer liver enzyme spikes compared to older azoles. These drugs could replace the riskiest ones within five years.
What Should You Do Now?
If you’re currently taking an antifungal:- Check your last liver test date. If it’s been longer than 4 weeks, call your doctor.
- Know your baseline liver enzyme levels. Ask for a copy of your lab report.
- Keep a symptom journal: fatigue, nausea, appetite loss, dark urine.
- Never mix antifungals with alcohol or other liver-stressing drugs without talking to your pharmacist.
- If you’re on terbinafine for nail fungus and it’s been over 6 weeks, get tested-even if you feel fine.
If you’re about to start one:
- Ask: “Is there a safer alternative?” Fluconazole is often just as effective with lower liver risk.
- Ask: “Do I need a genetic test?” Especially if you’re on voriconazole or itraconazole.
- Ask: “What are the signs I should call you immediately?”
Antifungals save lives. But they’re not harmless. The risk is real, predictable, and preventable-with the right checks in place. Don’t assume your doctor knows. Don’t wait for symptoms. Take control. Your liver won’t tell you it’s in trouble until it’s too late.
Can antifungals cause permanent liver damage?
Yes, in rare cases. While most liver injuries from antifungals reverse after stopping the drug, some patients develop acute liver failure requiring transplant. Ketoconazole and voriconazole have the highest rates of severe injury. Early detection and stopping the drug can prevent permanent damage, but delays increase the risk of irreversible harm.
Is terbinafine safe for long-term use?
Terbinafine is generally low-risk, but not risk-free. The FDA warns of rare but serious liver failure. Monitoring is recommended at 4-6 weeks and then every 4-6 weeks if treatment lasts beyond 8 weeks. Most liver issues appear within the first 6 weeks, but cases have been reported as late as 12 weeks. Never skip blood tests just because you feel fine.
Why is ketoconazole still available if it’s so dangerous?
Ketoconazole is still available in the U.S. but only for rare, life-threatening fungal infections like endemic mycoses-when no other antifungal works. It’s banned for skin and nail infections. The FDA restricted it in 2013 after hundreds of liver injury reports, including deaths. It’s no longer sold over the counter and is rarely prescribed outside specialized centers.
Can I take antifungals if I have fatty liver disease?
It depends. Fatty liver disease increases your risk of drug-induced liver injury. Fluconazole is often preferred over itraconazole or voriconazole in these cases. Your doctor should check your liver function before and during treatment. Some experts avoid azoles entirely in advanced fatty liver and use echinocandins or topical treatments instead.
Do over-the-counter antifungals affect the liver?
Topical antifungals-creams, sprays, powders for athlete’s foot or yeast infections-do not affect the liver because they’re not absorbed into the bloodstream. Only systemic antifungals (pills or IV drugs) carry liver risks. Never confuse topical treatments with oral or injectable versions.
What’s Next?
If you’re on an antifungal, the next step is simple: check your labs. Call your doctor or pharmacy and ask for your most recent liver test results. If you haven’t had one in the last month, schedule one. Write down your symptoms-even the small ones. Bring them to your appointment.If you’re not on one yet but might need one, ask your doctor: “What’s the safest option for my liver?” Don’t accept “It’s fine” as an answer. Demand specifics. Know your options. Your liver doesn’t have a voice-but you do.

Glendon Cone
December 31, 2025 AT 02:09Bro, this is the kind of post that saves lives. I’m a pharmacist and I’ve seen too many patients on terbinafine with zero LFTs. One guy showed up with jaundice and thought it was ‘just dehydration.’ Dude, your liver doesn’t text you first. Get tested. Period. 🩺
srishti Jain
December 31, 2025 AT 13:24Stop prescribing antifungals like candy. People die from this.
Hayley Ash
January 1, 2026 AT 14:49Wow so now we’re blaming doctors for not ordering blood tests? What’s next, mandatory yoga before taking a pill?
Kelly Gerrard
January 2, 2026 AT 14:19As a medical professional with over 20 years in hepatology I must emphasize that the data presented here is not only accurate but grossly underreported. The FDA's passive surveillance system misses 90% of DILI cases. We are in a silent epidemic. Patients are not being warned. Providers are not being educated. And the pharmaceutical industry continues to profit while people’s livers fail. This is not a matter of personal responsibility. This is systemic negligence. If you are on any systemic antifungal and your doctor has not ordered a baseline LFT within 72 hours of prescribing, you are being put at unacceptable risk. Demand your rights. Your life is not a clinical trial.
Aayush Khandelwal
January 4, 2026 AT 09:32Let’s talk CYP450 polymorphisms. The CYP2C19 poor metabolizer phenotype is rampant in South Asia - up to 30% of Indians are homozygous. Voriconazole clearance drops like a rock. I’ve seen patients on 200mg daily with levels spiking to 25 mcg/mL (toxic > 5). Yet we’re still prescribing like it’s 2010. We need point-of-care genotyping. Not ‘maybe someday.’ Now. This isn’t sci-fi - it’s pharmacokinetics 101.
Sandeep Mishra
January 4, 2026 AT 15:27There’s a quiet dignity in listening to your body. Fatigue isn’t just ‘being tired.’ Jaundice isn’t ‘yellow skin.’ These aren’t side effects - they’re signals. We’ve forgotten how to listen. We rush to fix, not to understand. If your doctor doesn’t take your symptoms seriously, find one who does. Your liver doesn’t have a mute button. Neither should you.
Colin L
January 5, 2026 AT 23:40Look, I get it, you’re scared of pills, but let’s be real - you’re probably one of those people who thinks ‘natural remedies’ are safer, right? Like tea tree oil on your toenails? Let me tell you about the 37-year-old woman I saw last month who developed fulminant hepatitis after using ‘organic antifungal spray’ she bought on Etsy. It had undiluted clove oil and turpentine. No regulation. No testing. No FDA. Just a woman with a blog and a PayPal account. So tell me again - who’s the real danger here? The FDA-approved drug with monitoring protocols or the unregulated hooch your wellness influencer sold you? The truth is, we’ve outsourced our responsibility to Google and Instagram. And now we’re paying with our livers.
Joseph Corry
January 7, 2026 AT 03:12Interesting how this post weaponizes fear under the guise of ‘awareness.’ The real issue isn’t the drugs - it’s the collapse of medical epistemology. We’ve replaced clinical judgment with algorithmic checklists. LFTs every week? That’s not medicine - it’s compliance theater. The real risk is overmedicalization. The liver is resilient. Most enzyme elevations are transient. We’ve turned patients into data points and doctors into lab technicians. Where’s the nuance? Where’s the trust? The real tragedy isn’t antifungal toxicity - it’s the erosion of the doctor-patient relationship.
Henry Ward
January 8, 2026 AT 03:41You people are pathetic. You’re so scared of a pill that you’d rather die of a fungal infection than risk your liver. Ketoconazole killed 1 in 500? So what? That’s less than your chance of dying in a car crash on the way to the pharmacy. Stop being drama queens. If you’re too weak to handle a little hepatotoxicity, maybe you shouldn’t be alive. The world doesn’t owe you a safe pill. It owes you responsibility. Take the drug. Get tested. Shut up. Or don’t. Your liver’s not my problem.
Kelly Gerrard
January 9, 2026 AT 09:39Henry, your comment is exactly why this crisis persists. You don’t understand medicine. You don’t understand risk. You think ‘tough it out’ is wisdom. It’s ignorance. I’ve seen patients die from this. Not because they were weak - because they were ignored. Your attitude kills. And you’re not brave - you’re dangerous.