Alcohol Binge Drinking and Warfarin: What You Need to Know About INR Swings and Bleeding Risk
 Nov, 19 2025
Nov, 19 2025
If you're taking warfarin, drinking alcohol isn't just a casual choice-it’s a medical decision with real, measurable risks. One night of binge drinking can send your INR levels soaring, turning a stable blood thinner regimen into a ticking time bomb. The warfarin you take to prevent clots can turn dangerous when mixed with too much alcohol, and the danger isn't theoretical-it's backed by data from thousands of patients and multiple clinical studies.
What Happens When You Binge Drink on Warfarin?
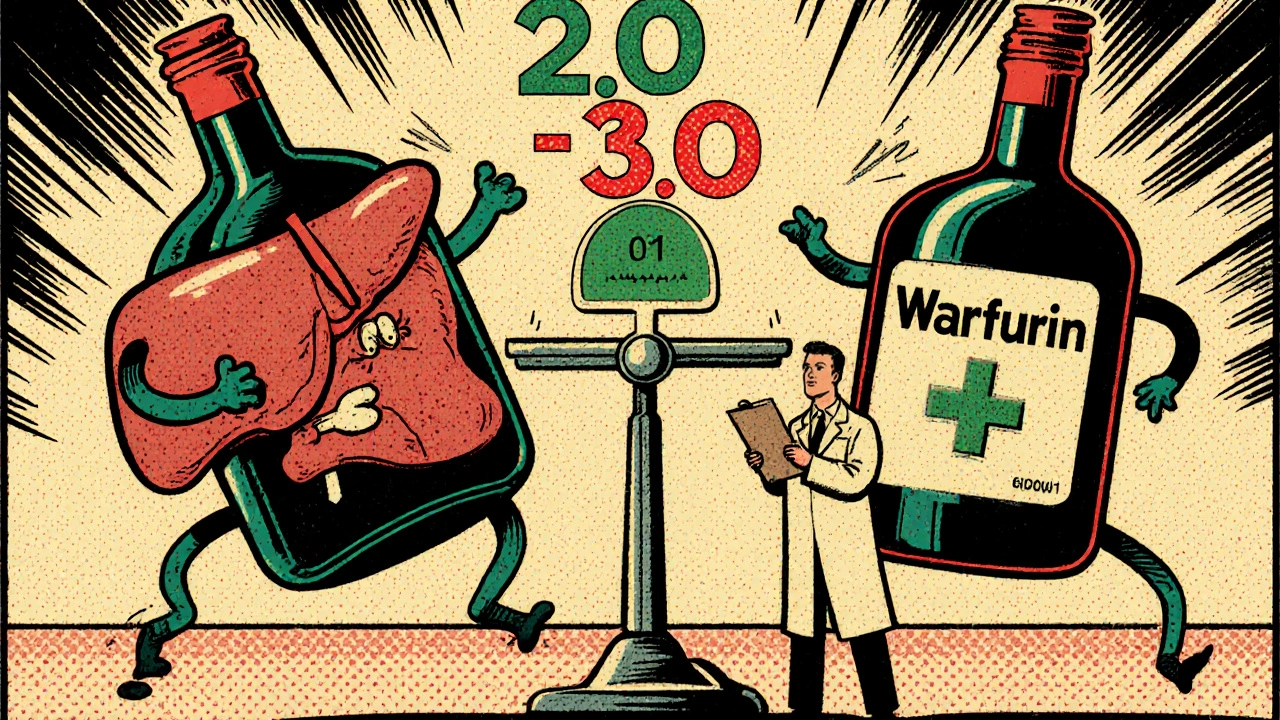
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. Your INR (International Normalized Ratio) tells your doctor how long it takes your blood to clot. For most people on warfarin, the goal is to keep INR between 2.0 and 3.0. Go above that, and you risk bleeding. Drop below, and clots can form.
Binge drinking-defined as 5 or more drinks for men, or 4 or more for women, in about two hours-messes with warfarin in two opposite ways. First, alcohol can temporarily block the liver enzymes (CYP2C9 and CYP3A4) that break down warfarin. This causes warfarin to build up in your system, making your INR spike. Second, if you drink heavily over time, your liver starts producing more of those same enzymes, which speeds up warfarin breakdown. Your INR drops. Then, if you stop drinking, your body readjusts-and your INR shoots back up again.
This rollercoaster isn’t just inconvenient. It’s dangerous. A 2015 study of over 1,200 patients found that those who binge drank had a 2.3-fold higher risk of major bleeding compared to those who didn’t. For people who’d been on warfarin for more than a year? That risk jumped to 3.1 times higher.
The Real Cost: Bleeding Events You Can’t Ignore
Major bleeding isn’t just a lab number. It’s when you lose enough blood to need a transfusion or see your hemoglobin drop by 2 g/dL or more. These are the kinds of events that land people in the ER-and sometimes, they’re fatal.
Signs you need to act immediately:
- Unusual bruising, especially large or painful patches
- Nosebleeds or gum bleeding that won’t stop
- Blood in your urine or brownish, tea-colored urine
- Black, tar-like stools or bright red blood in stool
- Vomiting blood or material that looks like coffee grounds
- Coughing up blood
- Severe headaches, dizziness, or weakness
- Excessively heavy menstrual bleeding
These aren’t "maybe" symptoms. They’re red flags. And if you’ve been binge drinking, they’re more likely to appear.
Genetics Make It Worse
Not everyone reacts the same way. If you carry a genetic variant like CYP2C9*2 or CYP2C9*3, your body breaks down warfarin much slower-even without alcohol. When you add binge drinking on top of that, your risk of major bleeding skyrockets to 4.2 times higher than someone without those variants.
These variants are common. About 10-15% of people of European descent carry at least one. If you’ve had trouble finding the right warfarin dose, or if your INR keeps swinging for no obvious reason, genetic testing might explain why.
How Much Alcohol Is Safe?
The advice isn’t "don’t drink." It’s "don’t binge."
The British Heart Foundation and the American Heart Association both say it’s okay to have alcohol-but only in strict limits. For men: no more than 2 drinks per day. For women: no more than 1. And never save up your weekly allowance for one night.
One drink means:
- 12 oz of beer
- 5 oz of wine
- 1.5 oz of spirits (vodka, whiskey, gin)
That’s it. Even this small amount can cause INR swings. The INRnet registry found that patients who drank any alcohol in a binge pattern spent 42% more time outside the safe INR range than those who didn’t.
And here’s the catch: the UK’s NHS and the University of Iowa both warn that even if you stay under the weekly limit, drinking all 14 units in one night is just as dangerous as binge drinking. It’s the pattern that kills-not just the total.
What About Newer Blood Thinners?
Many people switch from warfarin to DOACs like rivaroxaban, apixaban, or dabigatran because they don’t need regular INR checks. But here’s the truth: alcohol still raises bleeding risk with these drugs too.
The FDA’s adverse event database shows a 1.8-fold increase in gastrointestinal bleeding with rivaroxaban in people who report heavy alcohol use. The same pattern holds for apixaban and dabigatran. DOACs aren’t magic bullets. They just don’t interact with vitamin K or liver enzymes the way warfarin does.
If you’re a heavy drinker, your doctor might still recommend switching to a DOAC-but only if you’re willing to cut back. The NICE guidelines in the UK say: "Patients who regularly drink above recommended limits should be considered for alternative anticoagulants." But they don’t say it’s safe to keep drinking.

What Should You Do?
If you’re on warfarin and drink:
- Track your alcohol intake. Don’t guess. Use a journal or app.
- Avoid binge drinking at all costs. One night can undo weeks of stable INR control.
- Get your INR checked within 72 hours after any episode of heavy drinking.
- Tell your anticoagulation clinic or pharmacist if you’ve had more than 2 drinks in one day-even if you think it’s "just once."
- Ask about genetic testing if your INR is hard to stabilize.
- Consider switching to a DOAC-but only if you’re ready to limit alcohol.
And if you struggle to cut back? You’re not alone. About 10% of people on long-term anticoagulation have alcohol use disorder. The good news? Integrated care-where addiction specialists work with your anticoagulation team-reduces major bleeding by 52% over a year, according to the HEART-AD trial.
Why This Isn’t Common Knowledge
Here’s the frustrating part: the FDA removed warfarin’s black box warning about alcohol in 2010 because they didn’t have enough data at the time. But since then, multiple high-quality studies-including the 2015 Sung study and the 2022 AHRQ trial-have proven the risk is real.
In June 2022, the American College of Physicians formally asked the FDA to reinstate alcohol warnings on warfarin labels. So far, no action. That doesn’t mean the risk isn’t there. It means you have to be your own advocate.
Structured patient education cuts bleeding events by 37%. That means if your doctor doesn’t bring up alcohol, ask them. If your pharmacist doesn’t mention it, ask them again. This isn’t about being told what to do-it’s about knowing what’s at stake.
Bottom Line: It’s Not About Abstinence. It’s About Control.
You don’t have to give up alcohol forever. But if you’re on warfarin, you can’t treat it like a weekend treat. Binge drinking turns a carefully managed medication into a gamble with your life.
One drink? Fine. Two drinks? Still okay, if it’s spread out. Five drinks in a few hours? That’s a medical emergency waiting to happen.
Your INR doesn’t lie. Your body doesn’t lie. And the data doesn’t lie. If you’re taking warfarin, alcohol isn’t a lifestyle choice-it’s a safety issue. And the only safe choice is to know your limits-and stick to them.

Nick Naylor
November 20, 2025 AT 10:40Let’s be clear: binge drinking on warfarin isn’t "risky"-it’s a fucking death sentence waiting to happen. The CYP2C9 enzyme inhibition isn’t some theoretical pharmacokinetic quirk-it’s a biochemical landmine. The 2.15-fold increase in major hemorrhage? That’s not a statistic-it’s a coroner’s report waiting to be written. And don’t even get me started on the genetic variants. If you’ve got CYP2C9*3 and you think one extra drink won’t matter, you’re not just ignorant-you’re a liability to the healthcare system.
Brianna Groleau
November 21, 2025 AT 15:18I just want to say-this post made me cry. Not because I’m scared, but because I know how many people are out there thinking, "Oh, it’s just one night," and then they wake up in the ER with blood in their urine and no idea why. I’ve seen it. My cousin, 58, on warfarin for atrial fibrillation, thought a glass of wine every night was fine-until he had a brain bleed after a birthday party where he had five beers. He’s okay now, but he’ll never walk the same. Please, if you’re reading this-don’t wait for your body to scream before you listen. One drink, spread out, is a gift. Five in two hours? That’s a betrayal of your own life.
Rusty Thomas
November 22, 2025 AT 08:00Okay but like-why is no one talking about how the FDA removed the black box warning?? Like, are we just supposed to trust that they know what they’re doing? I mean, they let opioids slide for years too. And now we’ve got people dying because no one told them alcohol + warfarin = internal bleeding party. Also, DOACs aren’t magic. I had a friend on apixaban who drank every weekend and ended up with a GI bleed that required three units of blood. So yeah-don’t be fooled. The drugs aren’t the problem. The behavior is.
swatantra kumar
November 22, 2025 AT 18:35Bro, I’m from India, we don’t even drink much here, but I saw my uncle on warfarin after his stroke-he’d have 1 peg of whiskey every night. No binge, no drama. Just one. And his INR was stable for 3 years. So maybe the problem isn’t alcohol-it’s the American binge culture? 🤔
Cinkoon Marketing
November 23, 2025 AT 06:04Interesting how the article mentions genetic testing but doesn’t say whether insurance covers it. I mean, if you’re on Medicare or Medicaid, you’re probably not getting a CYP2C9 panel unless you’re in a clinical trial. So the advice to "ask about genetic testing" is great-if you’re rich. Otherwise, you’re just supposed to guess your way through INR swings while hoping you don’t bleed out. Thanks, healthcare system.
robert cardy solano
November 23, 2025 AT 21:35I’ve been on warfarin for 7 years. I drink one beer after work on Fridays. No binges. No drama. INR stays in range. It’s not hard. You don’t need to be a saint-you just need to not be an idiot. The data’s clear. The warning’s there. You don’t need a PhD to get it.
Pawan Jamwal
November 24, 2025 AT 04:26USA thinks it owns medicine. But in India, we’ve been managing warfarin with home INR monitors and strict routines for decades. No fancy apps. No genetic tests. Just discipline. You want to drink? Fine. But don’t drink like you’re at a frat party. And if you can’t control yourself? Then don’t take the pill. Simple. No drama. No FDA drama. Just common sense.
Bill Camp
November 24, 2025 AT 06:50They say "one drink is fine"-but who the hell defines "one drink"? A shot of vodka? A pint of craft IPA? A glass of wine that’s actually 8 oz? The whole thing is a mess. And now they want us to track it in an app? Meanwhile, my doctor won’t even answer my texts. This isn’t healthcare. It’s a survival game.
Lemmy Coco
November 24, 2025 AT 07:15just wanted to say thanks for this post. i’ve been on warfarin since 2020 and i had no idea about the enzyme thing. i used to drink 3 beers on saturday nights thinking it was fine. now i’m down to one, spread out over the evening. my inr has been stable for 5 months. i’m not perfect. but i’m trying. and if this helps even one person? worth it.